(UroToday.com) The 2024 Advanced Prostate Cancer Consensus Conference (APCCC) meeting featured a session on the management of metastatic hormone-sensitive prostate cancer (mHSPC), and a presentation by Dr. Maria De Santis discussing the management of frail patients with mHSPC. Frailty is defined as an aging-related state, resulting from a decrease in physiological reserves of multiple systems, which increases vulnerability to stressors. Patients are considered “pre-frail” if they have 2 of 5 components and frail if they have >= 3 of 5 of the following components:
- Nutrition: unintentional weight loss of body mass index < 18.5 kg/m2
- Energy: positive answer to the question “Do you feel weak now?” or negative answer to the question “Do you have a lot of energy?”
- Physical activity: low level of activity according to the IPAQ questionnaire (self-reported instead of measures of grip strength and slow walking speed)
- Physical strength: difficulty lifting a bag weighing 5 kg
- Mobility: difficulty walking up and down the stairs
Dr. De Santis notes that the life expectancy of frail men is a median of 1.2 years (95% CI 1.0-1.5) and the life expectancy of pre-frail men is a median of 6.0 years (95% CI 5.5 – 6.5). There are many mortality risk calculators available including the Schonberg Index and the Lee Index. Additionally, there are several ways to diagnose frailty, but Dr. De Santis favors the following algorithm, which incorporates G8 screening and a comprehensive geriatric assessment: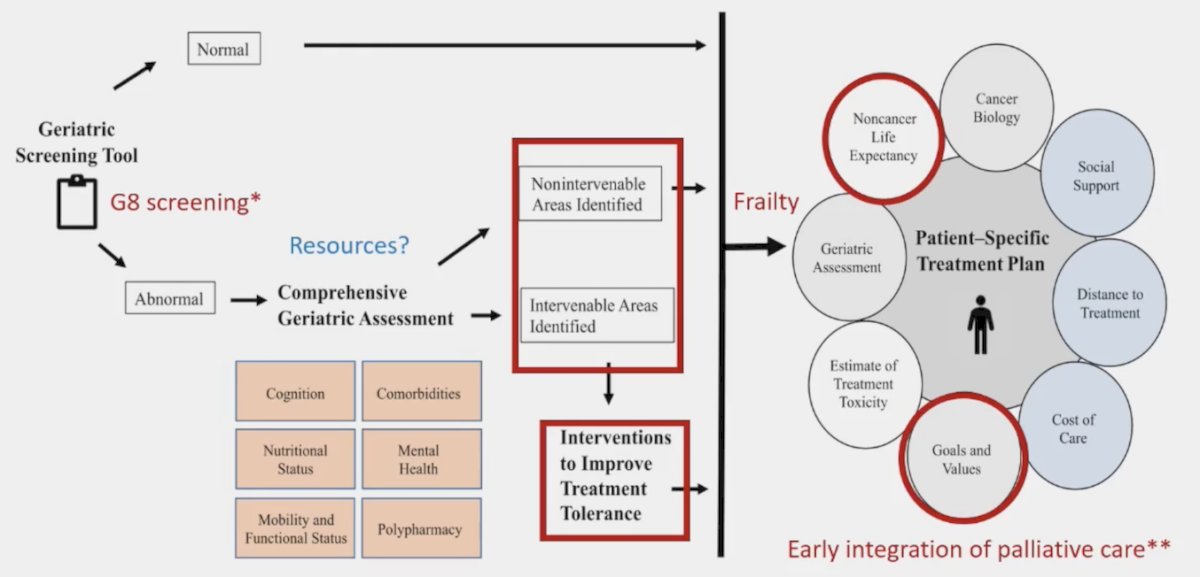
From a clinical perspective, frailty is a potentially reversible condition, however in the mHSPC setting, is there time for interventions to improve the frailty status? From a guidelines standpoint, the EAU states that for first-line treatment of mHSPC, we should “not offer ADT monotherapy to patients whose first presentation is M1 disease if they have no contraindications for combination therapy and have a sufficient life expectancy to benefit from combination therapy (ie. >1 year) and are willing to accept the increased risk of side effects” (Strength rating: Strong).
Dr. De Santis then discussed the Francini et al.1 study that assessed whether a classification based on time of metastatic disease (after prior local therapy vs de novo) and disease volume (low volume vs high volume) are prognostic for mHSPC patients treated with ADT. Among 436 patients treated at the Dana Farber Cancer Institute included in the analysis, the median overall survival for patients after prior local therapy/low volume disease was 92.4 (95% CI: 80.4-127.2) months and 43.2 (95% CI: 37.2-56.4) months for de novo/high volume disease, whereas intermediate values were observed for after prior local therapy/high volume disease and de novo/low volume disease. A robust gradient for both outcomes was observed (Trend test p < 0.0001) in the four groups: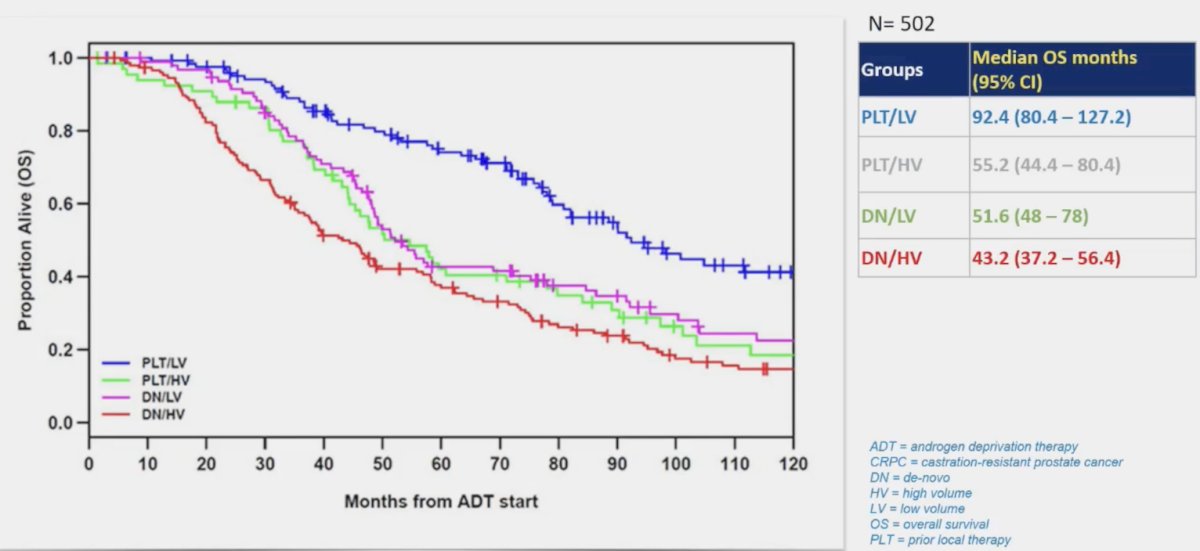
Additionally, time to CRPC is as follows: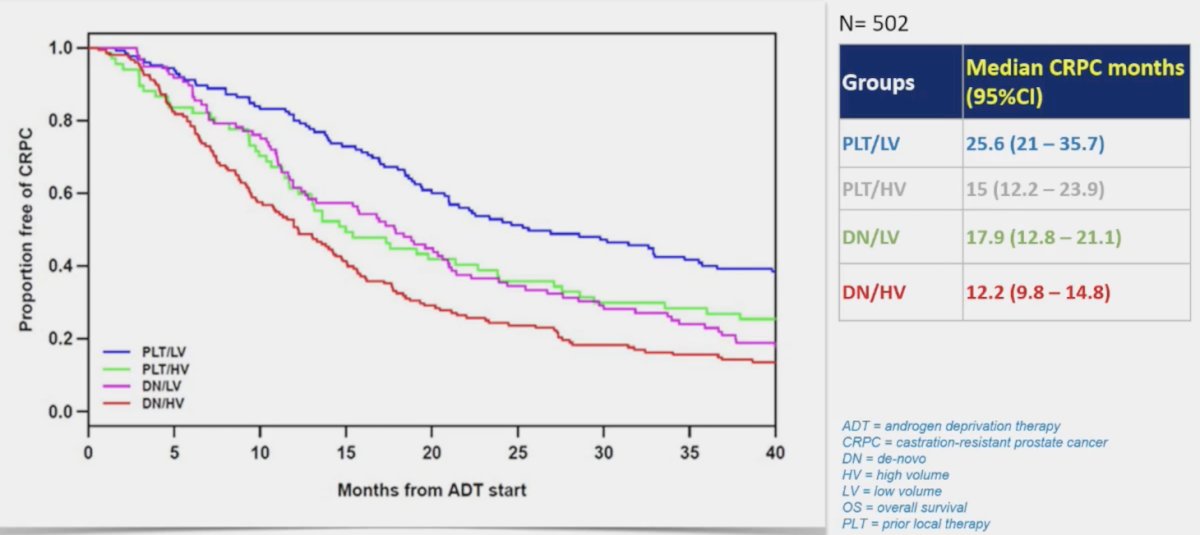
Rajwa and colleagues recently published a systematic review and meta-analysis assessing the effect of chronological age on overall survival among patients treated with combination therapies for mHSPC.2 Among 9 included randomized clinical trials and 9,183 patients, younger and older men constituted 51% and 49% of included patients, respectively. Docetaxel + ADT significantly improved overall survival among both older (HR 0.79, 95% CI 0.63-0.99, p = 0.04) and younger patients (HR 0.79, 95% CI 0.69-0.90, p < 0.001) with no differences according to age. Additionally, ARSI + ADT improved overall survival in older (HR 0.72, 95% CI 0.64-0.80, p < 0.001) and younger (HR 0.58, 95% CI 0.51-0.66, p < 0.001) patients, however, younger patients did benefit more (p = 0.02).
Dr. De Santis then presented a case of an 84-year-old male, frail (3/5 points), with mHSPC (de novo/high volume) and mild symptoms. His natural life expectancy was 3-4.5 years, he was on seven concomitant medications, including clopidogrel for atrial fibrillation and stroke prevention. His medical history also included hypertension and mild diabetes. Dr. De Santis noted that frailty rarely comes without polypharmacy and drug-drug interactions. In fact, for patients on 5-9 medications, there is a 50% chance of an adverse drug reaction. Drug-drug interactions are frequent and potentially harmful/life-threatening with stronger CYP3A4 inducers/inhibitors. Thus, abiraterone + prednisolone may be preferred over enzalutamide, apalutamide, or darolutamide. Referring back to the patient example, it is important to understand the patient’s goals: improve symptoms, no deterioration in health, and maintain quality of life. So, for this patient, triplet therapy is not an option and he would be treated with ADT +/- ARPI and potentially palliative radiotherapy to the bone or prostate.
Dr. De Santis provided the following list of interventions to improve tolerance of treatment and quality of life for men on ADT. These include bone health management, assessing fall risk, and maintaining adequate cardiovascular health: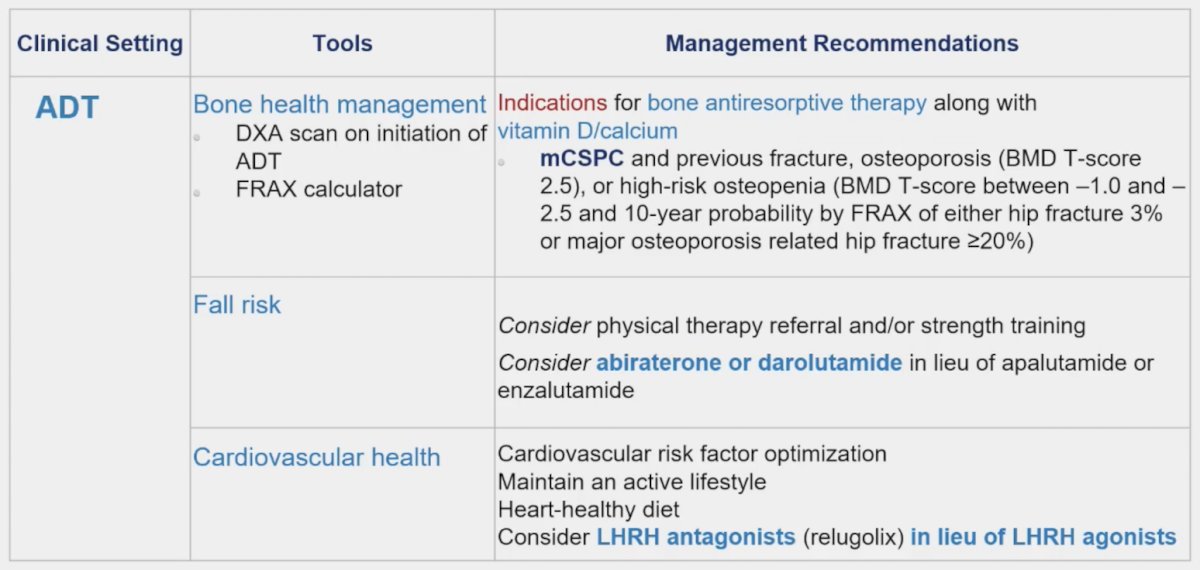
Dr. De Santis concluded her presentation discussing the management of frail patients with mHSPC with the following take-home messages:
- We need to explore frailty status, life expectancy, and goals with our patients
- Consider ADT alone in patients with a life expectancy of <= 1 year
- Continuous supporting interventions are crucial (physical therapy/training, osteoporosis prophylaxis)
- LHRH antagonists should be used if cardiovascular health is a priority
- We can consider the addition of an ARPI, with selection dependent on the side effect profile, risk of falls, and potential drug-drug interactions
- We should consider early palliative care involvement
Presented by: Maria De Santis, MD, PhD, Charité Universitätsmedizin, Berlin, Germany
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Advanced Prostate Cancer Consensus Conference (APCCC) Meeting, Lugano, Switzerland, Thurs, Apr 25 - Sat, Apr 27, 2024.
References:
- Francini E, Gray KP, Xie W, et al. Time of metastatic disease presentation and volume of disease are prognostic for metastatic hormone-sensitive prostate cancer (mHSPC). Prostate. 2018 Sep;78(12):889-895.
- Rajwa P, Yanagisawa T, Heidegger I, et al. Association between age and efficacy of combination systemic therapies in patients with metastatic hormone-sensitive prostate cancer: A systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2023 Mar;26(1):170-179.


