(UroToday.com) In a moderated poster presentation at the 2022 American Urologic Association Annual Meeting held in New Orleans and virtually, Dr. Naiki presented an analysis of abiraterone and bicalutamide (each with androgen deprivation therapy (ADT)) in metastatic castration-sensitive prostate cancer (mCSPC). The LATITUDE and STAMPEDE trials demonstrated that, compared to placebo + ADT alone, the addition of abiraterone was associated with improved overall survival. However, unlike the ENZAMET trial, an active comparator was not used. In Japan, bicalutamide (Bica) and ADT (combined androgen blockade: CAB) is frequently provided for mCSPC. Thus, these authors performed a retrospective comparison of these two treatment paradigms.
To do so, they identified 178 patients with high-risk mCSPC using the LATITUDE definition across multiple institutions of the Tokai Urologic Oncology Research Seminar. Among these 178 men, 103 had received ADT plus upfront abiraterone (abiraterone group) and 75 had received ADT plus bicalutamide (bicalutamide group). Kaplan–Meir analysis was used to retrospectively analyze survival and cancer recurrence. Univariate and multivariate Cox regression analyses identified potential prognostic factors for progression-free survival (PFS). To adjust for differences in baseline characteristics, the authors used a propensity score matched analysis.
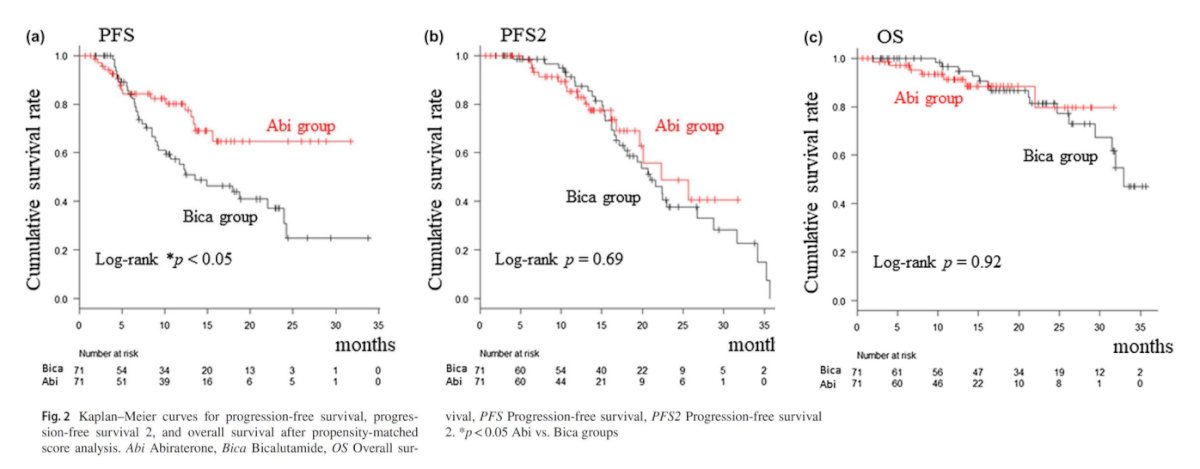
Interestingly, the authors did not observe significant differences in major clinicopathological characteristics between the two groups. However, the rate of castration resistant prostate cancer (CRPC) development was higher among patients treated with bicalutamide compared to abiraterone (50.6% vs. 25.2%, p<0.001). Further, the median PFS was significantly longer among patients receiving abiraterone (not reached) compared to those in the bicalutamide group (13.6 months; 95% CI: 9.2–22.2) (p<0.001). Further, time to second progression was also superior among patients receiving abiraterone (p=0.07).
Using both univariate and multivariate analyses, Gleason pattern 5, high alkaline phosphatase levels, and treatment with conventional CAB using bicalutamide were significantly associated with short PFS.

Similar results were found when the authors used a propensity score matched cohort with development of CRPC significantly more common among those treated with bicalutamide (49.3% for bicalutamide group vs. 23.9% for abiraterone group, p<0.01) and median PFS significantly shorter (13.6 months, 95% CI: 9.1–24.0 vs not reached, 95% CI: 15.6–NA, p<0.05).
Thus, the authors conclude that these real world data demonstrated that the upfront use of abiraterone in addition to ADT is associated with improved oncologic outcomes compared to conventional combined androgen blockade with bicalutamide in patients with LATITUDE high-risk mCSPC.
Presented by: Taku Naiki, MD, PhD, Associate Professor, Nagoya City University Graduate School of Medical Sciences

