(UroToday.com) The 2022 American Urological Association (AUA) Annual Meeting featured work from Mr. Kostantinos Morris and colleagues from Duke University School of Medicine (Durham, North Carolina) assessing the usage of prostate health index (PHI) in pre-biopsy work-up of African-American men.
Currently, prostate cancer (PCa) screening remains to be a grey zone with numerous knowledge gaps. The current screening tools available (PSA, ExosomeDx, and 4K) do not provide clear guidelines and thresholds for accurate and confident exclusion or detection of PCa. This lack of a clear threshold often contributes to patients’ hesitations towards undergoing prostate biopsy. Mr. Kostantinos Morris and colleagues specifically focused on African American men, a population that is at risk of having a greater baseline PSA, presenting with advanced disease, and having higher mortality rate and Gleason Grade Group (GGG) compared to white men with the same stage PCa. The biggest problem with prostate-specific antigen (PSA) and percent free prostate-specific antigen (%PSA) is their inability to accurately balance specificity and sensitivity of prostate cancer detection. PSA values in the “gray zone” of 4 to 10 ng/ml make it difficult to diagnose PCa; hence, prostate health index (PHI), calculated as PHI = p2PSA/Free PSA x √PSA has been FDA approved in 2012 to evaluate PCa amongst patients with PSA in the “gray zone”. Amongst patients with a Gleason score >/= 6, PHI has a higher predictive value and specificity than tPSA and % PSA
A total of 236 African American men with a PSA of 4-10 ng/mL, a PHI score, and a prostate biopsy between 2016 and 2020 were retrospectively identified and enrolled. Patients were stratified based on established PHI cutoffs: 0-26.9, 27-35.9, 36.0-54.9, and 55.0+. Multivariate logistical regressions were performed amongst the 4 groups to evaluate possible independent predictors of PCa. A chi-square analysis was conducted to assess the compliance with biopsy recommendations. The group with PHI of 0-26.9 served a reference group.
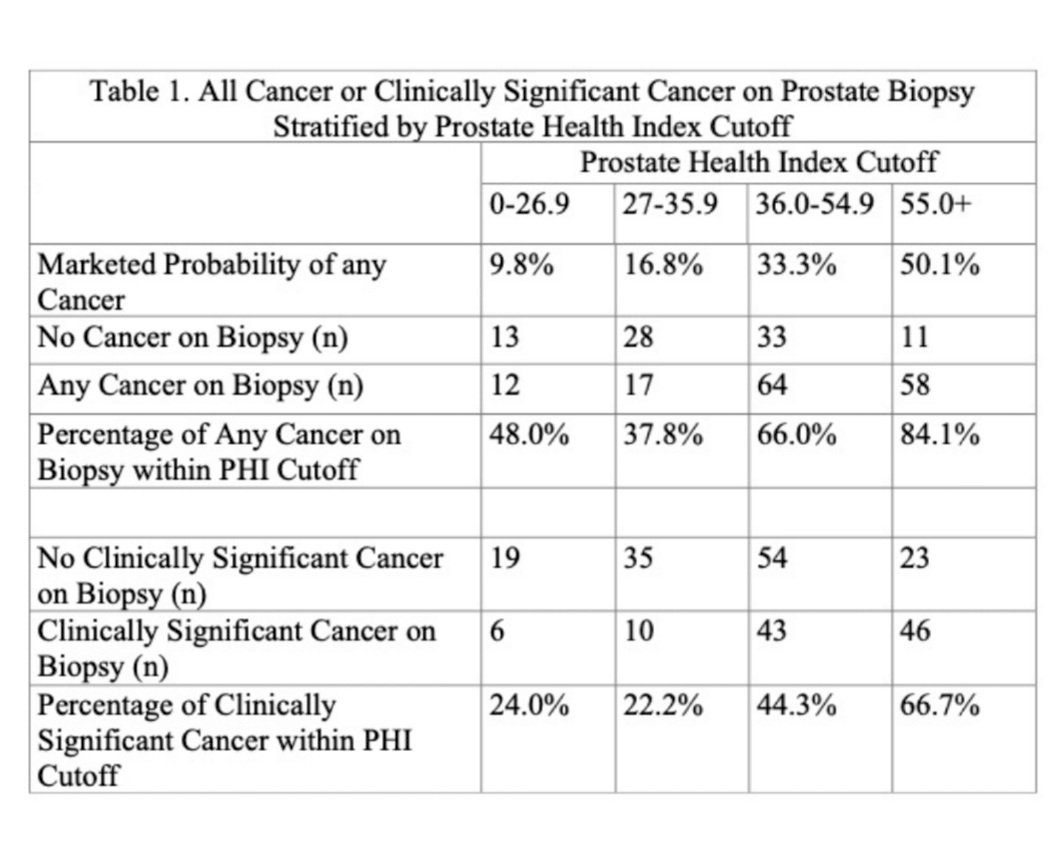
The mean PSA and PHI for all 236 subjects were 6.5 ng/ml and 48.5, respectively. The rate of PCa detection post-biopsy was 48%, 38%, 66%, and 84% for groups with PHI 0-26.9, 27-35.9, 36.0-54.9, 55.0+, respectively (Table 1). The overall detection rate at biopsy was 64.0% for all PCa. The overall rate of detection for clinically significant cancer (CSC), defined as Gleason = 7, was 44.5% and 24%, 22%, 44%, and 67% for groups with PHI 0-26.0, 27 – 35.9, 36.0 – 54.9, and 55+, respectively.
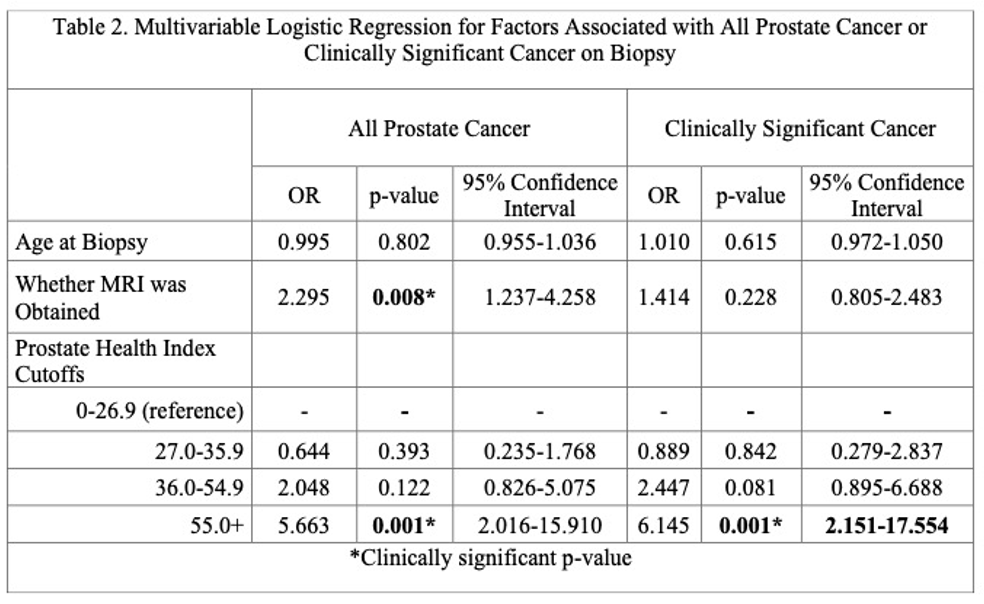
The identification of all PCa and CSC was only significantly associated with PHI 55+ on multivariate analysis (Table 2). Even when proposing a new cutoff of PHI 23.0 which corresponds to a 10% detection of CSC, only 5% of unnecessary prostate biopsies were avoided. A total of 358 biopsies were recommended with 292 (81.6) of biopsies completed. However, the compliance rate is limited by the lack of homogeneity among physicians when recommending biopsies.
Through this study investigating the role of PHI in pre-biopsy work-up of African-American men with PSA of 4 to 10 ng/mL, Mr. Kostantinos Morris and colleagues presented the following conclusions:
- The current PHI stratification is not useful for African-American men as seen by the elevated PCa detection across all four groups.
- PHI does not avoid unnecessary biopsies in the high-risk population, even with the proposed cutoff of PHI 23.0.
- PHI may be a helpful tool in increasing biopsy compliance in high-risk African American men.
Presented by: Kostantinos Morris, Division of Urology, Duke University School of Medicine, Durham, North Carolina
Co-Authors: Judd Moul, MD, Srinath Kotamarti, MD
Written by: Minh-Chau Vu, B.S., Department of Urology, University of California, Irvine during the 2022 American Urological Association (AUA) Annual Meeting, New Orleans, LA, Fri, May 13 – Mon, May 16, 2022.