(UroToday.com) The 2022 Annual Meeting of the American Urological Association (AUA) was host to The International Bladder Cancer Group (IBCG) AUA Bladder Cancer Forum which featured a case-based debate regarding the role of radical cystectomy in cN1-2 disease. This session was moderated by Dr. Kamal Pohar, and Dr. Yair Lotan was tasked with providing arguments against radical cystectomy in this setting.
Dr. Lotan began his presentation with the following key questions:
- Does negative imaging prior to cystectomy correctly identify patients who are pathologically node negative?
- After induction chemotherapy, is there a different outcome if a patient is pN0 or pN+?
- Does consolidative treatment improve survival?
Dr. Lotan emphasized that imaging is unreliable to assess nodal status. Both CT and MRI use the same metrics to indicate suspicious lymph nodes:
- Pelvic nodes: >8 mm
- Abdominal nodes: >10 mm
- Radiologic micro metastases are not detected (false negative)
- Nonpathologically enlarged lymph nodes (false positive)
A recent report published in Urologic Oncology evaluated the accuracy of CT scan in this setting. Of 130 patients identified as cN+, 76 (58.5%) received induction chemotherapy prior to radical cystectomy. A post-chemotherapy CT scan was obtained in those patients, and using a median node size of 8 mm cutoff:
- Sensitivity: 72%
- Specificity: 80%
- PPV: 87%
- NPV: 62%
Patients who were pN+ had:
- Greater median number of enlarged nodes (3 versus 1)
- Larger median size of the largest node (11.5 mm versus 10 mm)
- Both findings were not statistically significant
Each 1 mm increase in size of the largest node on post-chemo CT scan increased the chance of having pN+ disease by 1.57 (95% CI: 1.02-2.44).
A recent report by Meijer et al. in EJSO evaluated 152 patients with T3 and/or LN positive disease, who were treated with at least 2 cycles of induction chemotherapy and achieved complete clinical response:1
- Complete pathologic response: 62.5%
- Positive nodes: 37.5%
- Thus, the PPV of response evaluation based on clinical staging was 62.5% (95% CI: 47%-76%)
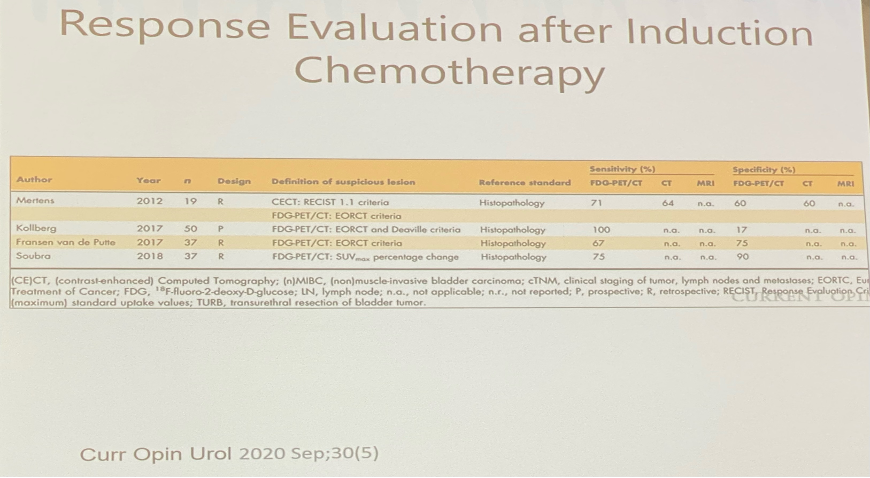
What about FDG-PET/CT to assess nodal status? A systematic review of 19 original reports evaluating the performance of FDG-PET/CT for lymph node assessment:
- Sensitivity 23-100%
- Specificity: 33-100%
FDG-PET/CT had superior sensitivity to conventional CT in 7 studies and equivalent sensitivity in 3 other studies. One study compared FDG-PET/CT to MRI and reported superior sensitivity and specificity of FDG-PET/CT (sensitivity: 33% vs 0%, specificity: 93% versus 80%). Differences in reported test performance are likely related to differences in:
- Size cut offs
- Short axis versus long axis
- Different SUVmax
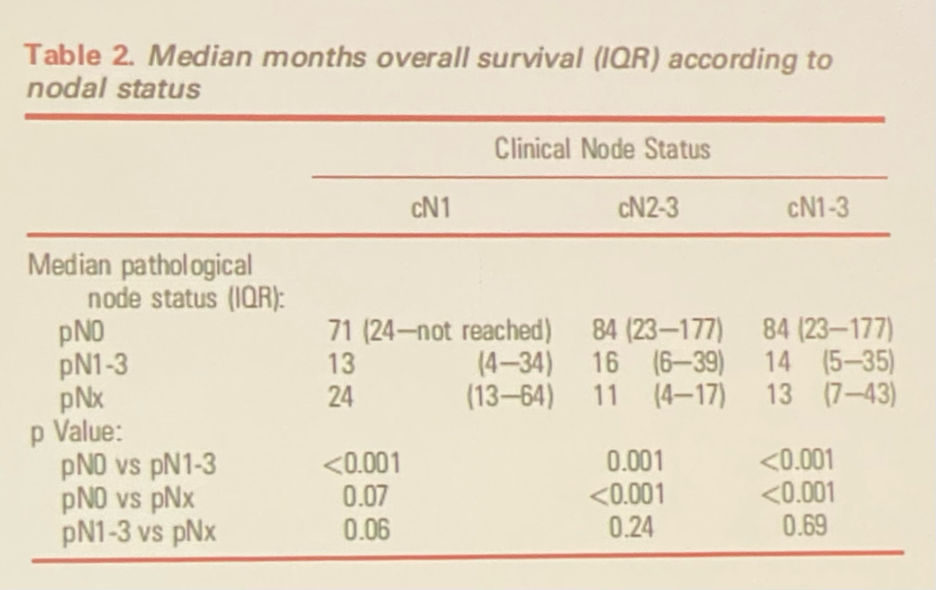
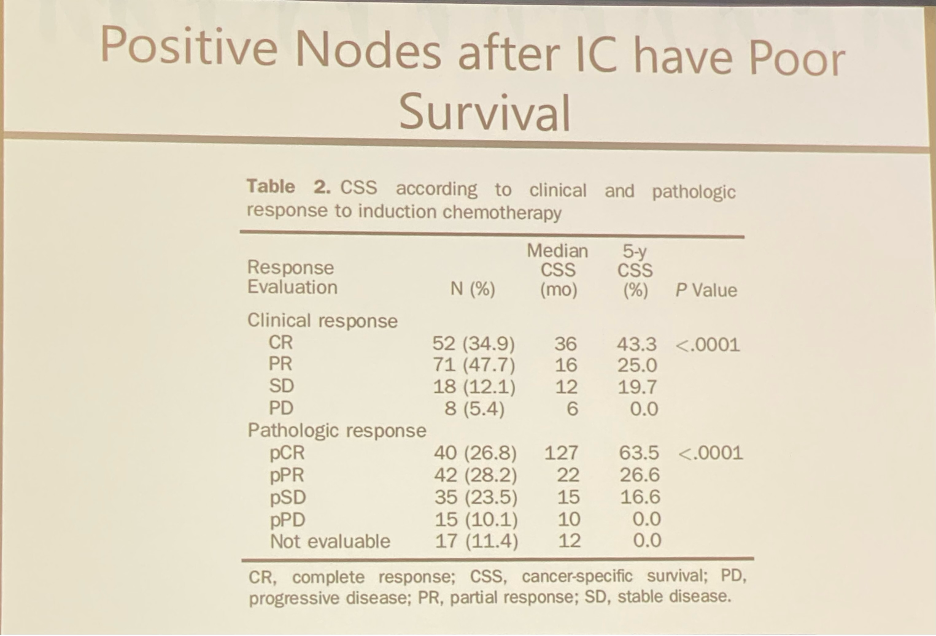
The next question is: After induction chemotherapy, is there a different outcome if a patient is pN0 versus pN+?
- Yes, much worse
In the same study by Meijer et al., patients with persistent ypN+ disease (n=33) had a median OS of 13 months (95% CI: 10-19 months) compared to a median OS of 27 months (95% CI: 28-58 months) for patients with pathologically node negative disease ypN0 (n=100). This is further elaborated on in the below Kaplan-Meier curve below:
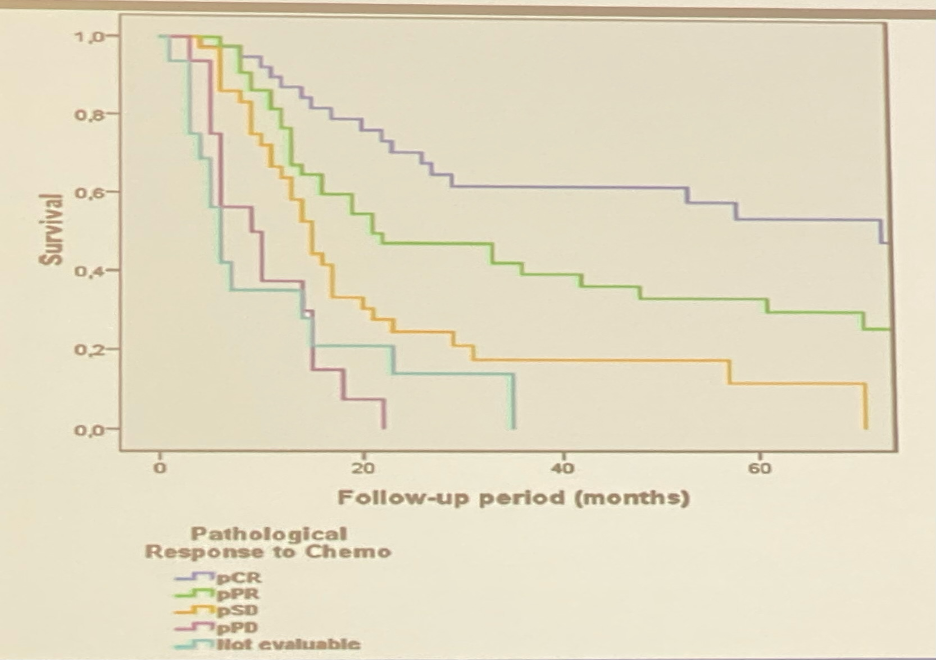
- 5-year OS: 53.8% for pCR and 33.4% for pPR (p<0.001)
- Patients with pathologically stable disease fared better than those with pathologically progressive disease
- Patients with pathologically progressive disease who underwent cystectomy had similar OS compared to the patients who were not operated
- These findings were confirmed in another series demonstrating that median OS for such patients is 10 months
What should one do with a patient with clinical N0 staging post-chemotherapy?
- If pN0, then maybe better survival with consolidation (No RCT available)
- Current imaging unreliable to distinguish pN0 from pN+
- Cystectomy is morbid and no clear benefit if pN+
Realistic options include:
- Take risk with cystectomy with best cure scenario of 30-40% cure
- Staging lymphadenectomy
- If pN0 then proceed with cystectomy, similar to what was performed previously with radical prostatectomies
- Can be performed via minimally invasive approaches easily with median retrieval of 10 LNs in the NCDB series
- Lymphedema rate of ~2% and complication rate between 9 and 11%
- Chemoradiation
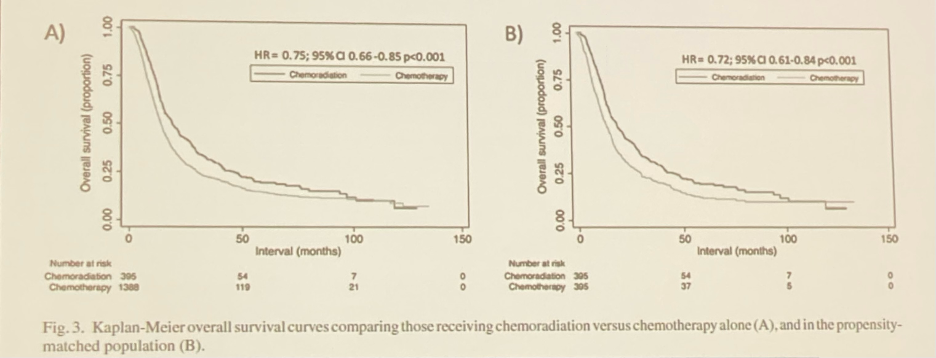
- Analysis from the NCDB (2004-13) for 1,783 patients diagnosed with cTanyN1-3M0 bladder cancer:
- 8% underwent chemotherapy alone
- 2% underwent chemoradiation alone
- Median OS 19.0 months versus 13.8 months in favor of chemoradiation
- Analysis from the NCDB (2004-13) for 1,783 patients diagnosed with cTanyN1-3M0 bladder cancer:
One must acknowledge the bias present in the literature:
- Compared with chemotherapy alone, radiotherapy was added for “higher-risk” disease:
- Older than 65 years
- More advanced T classification
- Non-urothelial histology
- Addition of radiotherapy to CT independently associated with improved survival in this “higher risk” cohort
- Use of cystectomy in the literature favors those who responded to chemotherapy and were healthier
Dr. Lotan re-addressed the questions raised at the beginning of the discussion:
- Does negative imaging prior to cystectomy correctly identify patients who are pathologically node negative?
- Not accurately
- After induction chemotherapy, is there a different outcome if a patient is pN0 or pN+?
- Yes, much worse if still pN+
- Does consolidative treatment improve survival?
- No RCTs (Node positive excluded from NAC trials)
- Only if pathologically complete response in nodes
Conclusions:
- Need better way to assess nodal status after induction chemotherapy
- Role of robotic lymphadenectomy for staging prior to decision on therapy needs to be evaluated
- Compare chemoradiation as alternative to cystectomy
- What is role of immunotherapy if persistent node positivity
Presented by: Yair Lotan, MD, Professor of Urology, Chief of Urologic Oncology, and holder of the Helen J. and Robert S. Strauss Professorship in Urology at UT Southwestern Medical Center
Written by: Rashid Sayyid, MD, MSc – Urology Chief Resident, Augusta University/Medical College of Georgia, @rksayyid on Twitter during the 2022 American Urological Association (AUA) Annual Meeting, New Orleans, LA, Fri, May 13 – Mon, May 16, 2022.
References:
Related Content: AUA 2022: Case Presentation: Is there a Role of Radical Cystectomy in cN1-2 Disease? Pro

