- Gleason 6 or below
- PSA density<0.15
- <3 cores involved
- <50% of any single core involved
The benefits of AS include avoiding over-treatment, avoidance of adverse effects of definitive therapy, maintenance of quality of life, and decreased initial costs. The disadvantages of AS include progression of the disease before therapy and a sacrificed opportunity for cure, making nerve-sparing surgery potentially contraindicated. Furthermore, there may be a need for adjuvant therapy in the form of radiotherapy or androgen deprivation therapy (ADT). Additionally, patients need to cope with anxiety due to the undertreated cancer, need for frequent monitoring and repeat biopsies, with their associated morbidity and cost. The is also lack of reliable biomarkers to predict progression.
The outcomes of AS after 10 years for low-risk PC and intermediate risk PC are 83.6%, and 68.4%, respectively. The PC specific survival for 10 years of low-risk PC and Intermediate risk PC is 98.2% and 95.5%, respectively. The risk of PC death was 3.75 times higher for intermediate risk than for low-risk disease (11.5% vs. 3.7%).
The follow-up trial for the pivot study, with 20 years follow-up comparing prostatectomy vs. observation, showed that surgery was not associated with significantly lower all-cause mortality or prostate cancer-specific mortality when compared to observation (Figure 1). Surgery was associated with a higher frequency of adverse events but a lower frequency of treatment for disease progression, mostly for asymptomatic, local, or biochemical progression. 1
Benson continued and asked the provocative question that given these results, why is radical prostatectomy still performed? The answer lies in the fact that the PIVOT trial had many flaws. These include:
- The original trial design required 2000 men to detect a 25% difference in survival.
- “Life expectancy of at least 10 years” was an entry criterion. However, at 10 years almost half the patients had died, leaving only 176 men in the surgery group and 187 in the observation group. By 15 years only 30% were alive.
- The study did not recruit healthy men who would be normal candidates for surgery. It only recruited elderly co-morbid men with a limited life expectancy
- Owing to patient selection flaws, only 11.4% of the deaths in the observation arm and 7.4% in the surgery arm were attributed to PC.
- Overall mortality is an appealing end-point, but if too many patients die from other causes, the majority of endpoints are non-informative for the comparison of interest
- The expectations of a 25% relative reduction in mortality when 85% of the events are non-informative requires an enormous treatment effect in the informative endpoints
- The finding that 1/5 of patients did not adhere to the assigned treatment further reduces the ability of the trial to discern a treatment effect
- According to Dr. Benson, this study never should have been accepted for publication and Dr. Benson recommends urologists not to sell their robot just yet…

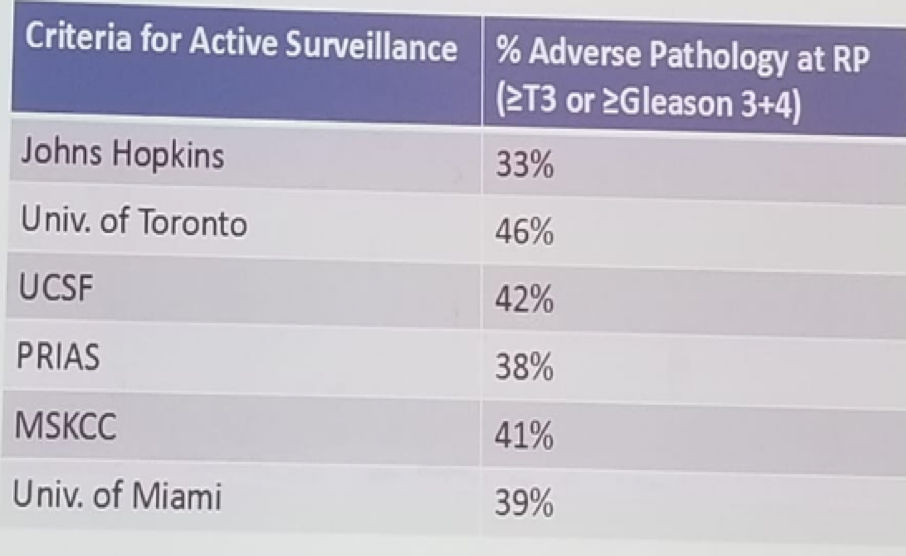
A 1/3 of men on AS may have higher risk features at the time of diagnosis of ‘low risk’ prostate cancer. Several studies have shown that 33-46% of patients on AS have >=T3 disease or Gleason 7 or above (Table 1). Re-biopsy should be standard for patients with a microfocus Gleason 4 or high-grade PIN on initial biopsy. The absence of cancer on immediate re-biopsy is predictive of the low likelihood of progression during follow-up.
Table 1 – Adverse features in patients on active surveillance:
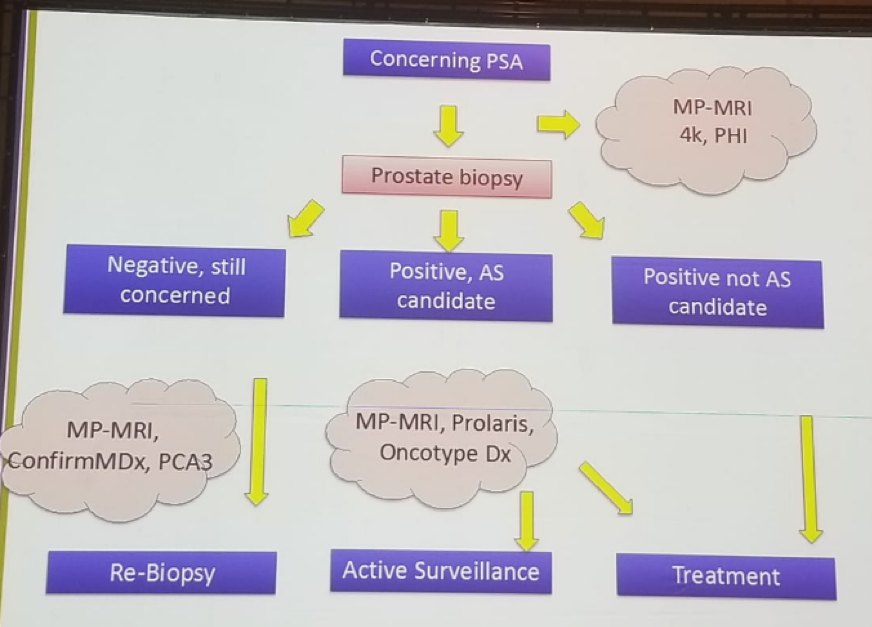
Benson summarized his talk with some points on the selection of patients for AS. Benson thinks that a single TRUS biopsy is unacceptable for AS entry, and a saturation biopsy should be performed. Additionally, restriction of eligibility criteria to more stringent biopsy characteristics will not eliminate the risk of unfavorable pathology at radical prostatectomy, but will significantly reduce the risk. Lastly, more studies are needed to identify the role of newer biomarkers, multiparametric MRI, and genomics in identifying the ideal AS patient. Dr. Benson concluded his talk with a proposed algorithm for AS used in Columbia University (figure 2).
Figure 2 – Proposed active surveillance protocol:
References:
1. Wilt TJ et al. NEJM 2017
Presented by: Mitchell C. Benson, MD, Columbia University, Irvine Medical Center, New York, NY, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel


