- Bladder carcinoma in situ (CIS)
- History of non-muscle invasive bladder cancer (NMIBC)
- CIS in the distal ureter
According to the AUA guidelines, follow-up of patients after RC should include:
- Chest imaging
- Cross-sectional imaging of the abdomen and pelvis with CT or MRI at 6-12 months intervals for 2-3 years and then annually
- CT urography or MRI urography of the abdomen and pelvis every 3-6 months for two years
- Chest imaging every 3-6 months for two years
- At year 3-5 CT/MR or PET and chest imaging annually
- At 6-10 years renal ultrasound annually
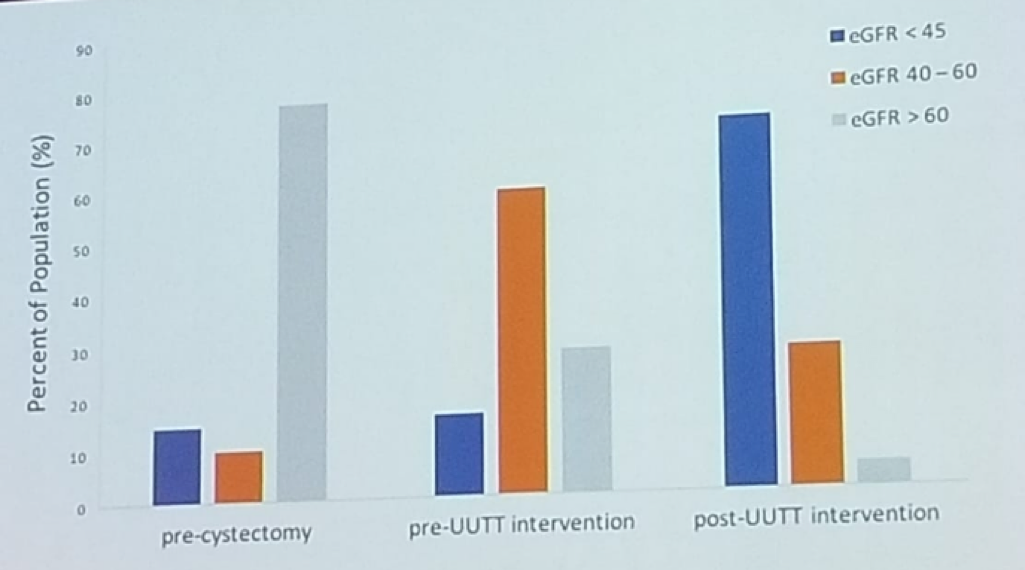
Figure 1 – EGFR reduction pre- and post- radical cystectomy:
The known risk factors for UTUC following RC include3:
- RC performed for CIS or NMIBC as CIS imposes a higher risk, and NMIBC is associated with a longer life expectancy.
- Positive ureteral margins (Odds ratio of 7.163, p<0.001)
- Prostatic urethra or membranous urethra involvement in women (Odds ratio 7.19, p<0.001)
- History of UTUC (Odds ratio of 7.25, p=0.03)
- The feasibility of retrograde ureteroscopy via ileal conduit and neobladder
- The anatomy of the afferent limb may restrict access in the neobladder
- Continent cutaneous diversion requires antegrade approach, however, percutaneous ureteral stent facilitates retrograde ureteroscopy.
Presented by: Seth Lerner, MD, FACS, Baylor College of Medicine, Houston, TX, USA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 FOIU 4th Friends of Israel Urological Symposium, July 3-5. 2018, Tel-Aviv, Israel
References:
1. Gakis et al. Eur Urol. 71:545, 2017
2. Fernandez, et al. Urol Oncol 30:821, 2012
3. Picozzini, et al. J Urol 188:2046, 2012


