There are other non-infectious IUC-related adverse effects that occur the longer an indwelling urinary catheter (IUC), particularly a transurethral IUC, is used for bladder drainage. They include catheter blockage, urine bypassing, bladder spasms, accidental catheter dislodgement, and non-deflating balloons.
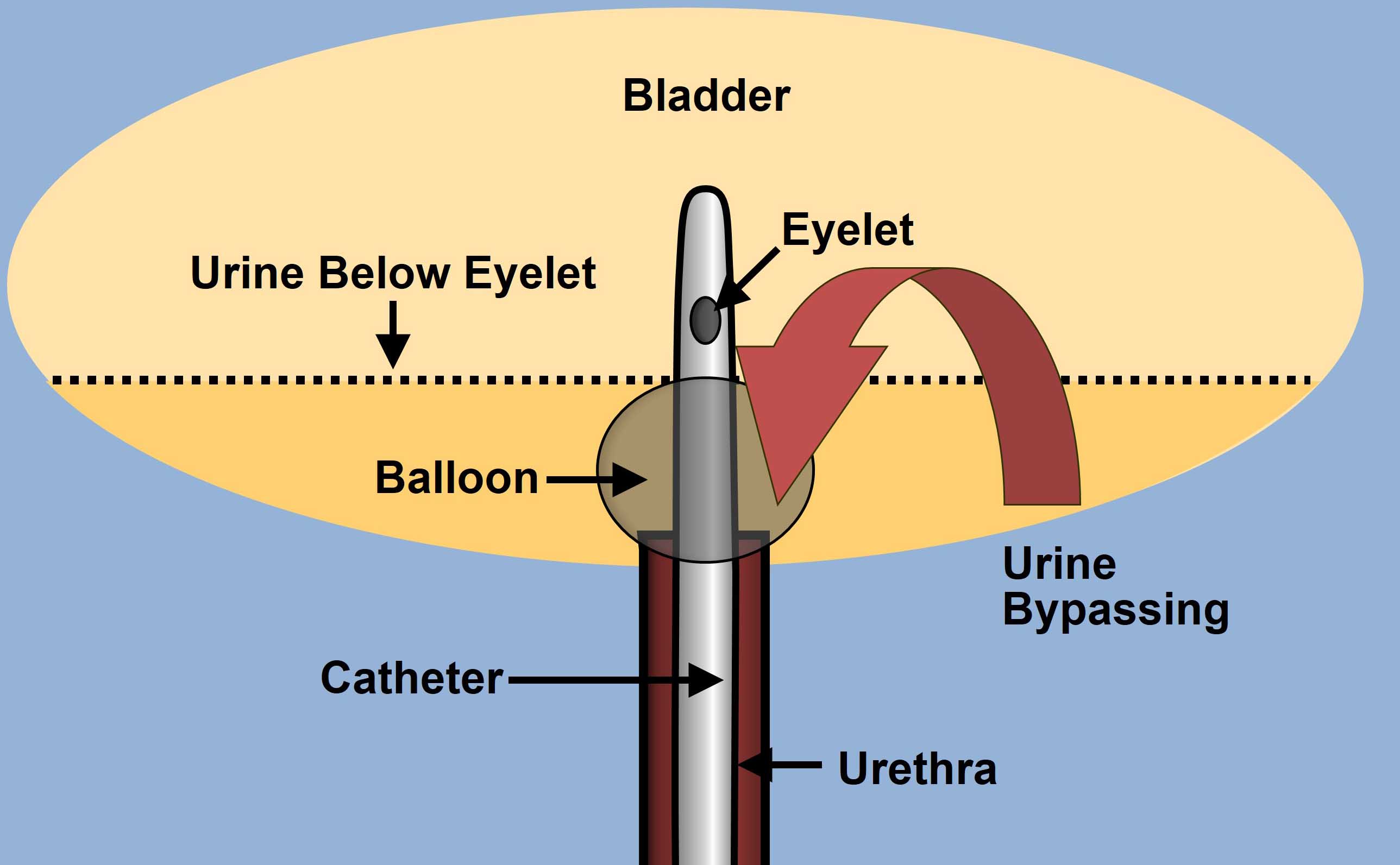
Hematuria is more likely to be seen in newly inserted catheters and in men, during insertion due to false passage in the prostatic urethra. Catheter blockage is more common in long-term IUC patients following the buildup of sediment in subclinical bacteriuria. A blocked catheter usually requires immediate catheter changes, often times leading to an unplanned visit by a home care nurse or a trip to the urology office or emergency room. Accidental IUC removal is more likely to be seen in residents of long-term care facilities or in home care patients than in acute care patients. Bypassing, which is when the bladder forces urine around either a transurethral or suprapubic (SP) catheter, has been reported to be as high as 79% in catheter users at home. A secondary analysis by Wilde et al (2017), of community-dwelling persons (n=193) with long-term IUCs, showed that leakage (bypassing) was reported at least once in last 12 months by 67% of patients. In this study, CAUTIs were marginally associated with catheter blockage but other catheter-related problems reported included blockage (34%), accidental dislodgment (28%), sediment (87%), bladder spasms (59%), kinks/twists (42%), and catheter pain (49%). Over 50% of patients report that an IUC is uncomfortable.
Patients who have recurring catheter-related adverse events should undergo diagnostic cystoscopy to determine the cause (e.g. stones, cancer). Patients should be screened yearly for bladder cancer if they have had an IUC for more than 10 years. Patients and caregivers should be educated about fluid intake, bowel management, hygiene and self-monitoring/management, including adverse events (Alex et al., 2020). The following table details nursing solutions for common IUC-related problems.
| Problem/Signs & Symptoms | Solution |
|---|---|
| Blockage: anything that inhibits or completely stops drainage of urine from the bladder through the catheter tube | |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Bypassing: urine leakage around catheter | |
|
|
|
|
|
|
|
|
| Inadvertent removal (unintended or accidental IUC extraction, catheter falls out) | |
|
|
|
|
|
|
|
|
|
|
| Pain or discomfort | |
|
|
|
|
| Difficult catheter removal | |
|
|
|
|
Table 1. CDC: Catheter-Associated Urinary Tract Infection
- IUC was in place for more than two days on the date of event, with day of device placement being day one, and an IUC was in place on the date of event or the day before. If an IUC was in place for more than 2 consecutive days in an inpatient location and then removed, the date of event for the UTI must be the day of device discontinuation or the next day for the UTI to be catheter-associated.
- Must have at least one of the following signs or symptoms
- Fever with temperature >38°◦C (if > 65 years of age, the IUC needs to be in place for more than 2 consecutive days in an inpatient location on date of “event”
- Suprapubic tenderness*
- Costovertebral angle pain or tenderness
- Urinary urgency+
- Urinary frequency+
- Dysuria+
- Patient has an aseptically obtained urine culture with no more than two species of organisms identified, at least one of which is a bacterium of > 105 CFU/ml.
Signs not directly associated with a CAUTI:
- Pyuria—not a good indicator as it is common in catheterized individuals
- Odor—the persistent bacteria in the urine of catheterized patients will produce odor
Possible signs in an elderly patient:
- Increased restlessness or altered mental status
- Change in health status not attributable to any other cause (pneumonia, medication side effects)
Treatment of CAUTI once a diagnosis is established:
- If possible, remove the catheter and follow bladder management at least until the antibiotic course is completed.
- If not possible to leave the catheter out, change the catheter prior to starting antibiotics so that there is the least amount of biofilm present.
- Start antibiotics—typical course of antibiotics is 7 to 14 days, usually a fluoroquinolone.
- Chart symptom improvement.
*With no other recognized cause
+ These symptoms cannot be used when a catheter is in place, but can be used if symptoms occur after urinary catheter removal, on the day of removal or day after removal
Adapted from CDC, Retrieved from https://www.cdc.gov/nhsn/pdfs/training/2019/cauti-508.pdf.
Published Date: October 2022