(UroToday.com) In a plenary session at the Society of Urologic Oncology Annual Meeting focused on early prostate cancer diagnosis and treatment, Dr. Neil Desai discussed the role of hypofractionation for patients treated with radiotherapy for unfavourable risk localized prostate cancer.
Dr. Desai first began by defining hypofractionation. While conventional radiotherapy utilizes treatments of 1.8 to 2 Gy per fraction delivered daily over 8 to 10 weeks, hypofractionation regimes use fewer, higher dose fractions. Prostate cancer in particular has a different cellular repair profile from a slower growth (as denoted with a lower alpha/beta ratio) which favours such an approach. Moderated hypofractionation is the use of 2.4 to 3.4 Gy per fraction while ultra-hypofractionation utilizes doses of 6 Gy or higher per fraction. The goal of hypofractionation is the reduce treatment burden and cost as well as potentially improve both efficacy and tolerability.
To this end, Dr. Desai cited a review encompassing a number of randomized controlled trials of moderate hypofractionation in prostate cancer. To date, this approach has been tested in approximately 6500 men within the confines of seven different randomized controlled trials. These trials have utilized multiple different treatment regimes across nearly all prostate cancer risk groups and found modest or no increased toxicity.
Dr. Desai cited the example of the CHHiP trial as an example. This RCT of more than 3200 men in the UK compared conventional fractionated treatment (74Gy/37#) with two hypofractionated regimes (57Gy/19# and 60Gy/20#), finding that 60Gy in 20 fractions was non-inferior to 74 Gy in 37 fractions in terms of biochemical control. However, he emphasized that long-term toxicity was not consistently different between these two treatment approaches, the patterns differed somewhat. Particularly, the peak in both bowel and urinary toxicity occurs earlier (and maybe somewhat more prevalent) in patients who received a hypofractionated regime.
Further, he emphasized that subgroup analyses according to prostate cancer risk group, patient age, tumor grade, tumor stage, and PSA level demonstrated that there is no evidence of harm with a hypofractionated approach.
Based on data such as these, moderate hypofractionation is now guideline endorsed across many guideline bodies including the NCCN; ASTRO, ASCO, and AUA; and EAU, EANM, ESTRO, ESUR, ISUP, and SIOG. This approach has benefits in terms of patient convenience, cost, and access to care while notably relying on the same radiotherapy technology.
The question then arises whether further hypofractionation can bring further benefit. Ultra-hypofractionation has been assessed for quite some time. There is long-standing data for this approach in the context of high-dose-rate brachytherapy. However, recent advances in radiotherapy technology and precision have introduced the potential for external beam stereotactic body radiotherapy. This approach has now been studied in two large, phase III randomized controlled trials.
Of these, the HYPO-RT-PCa trial is both larger and more mature. This study randomized nearly 100 men to a conventional regime of 78Gy in 39 fractions of 42.7 Gy in 7 fractions. Notably, patients in this non-inferiority RCT did not receive androgen deprivation therapy. The authors found comparable five-year failure-free survival though toxicity was somewhat worse in the ultra-hypofractionated group at 1 year. Dr. Desai emphasized that this trial utilized older radiotherapy techniques.
The more recent PACE-B trial demonstrated no difference in grade 2 or greater GI toxicity of biochemical progression-free survival between a 5 fraction ultra-hypofractionated regime and conventional or moderate hypofractionated treatment, though there were higher rates of grade 2 or greater GU toxicity (11.8% vs 5.8%). This was driven by a symptomatic flare at 12-18 months.
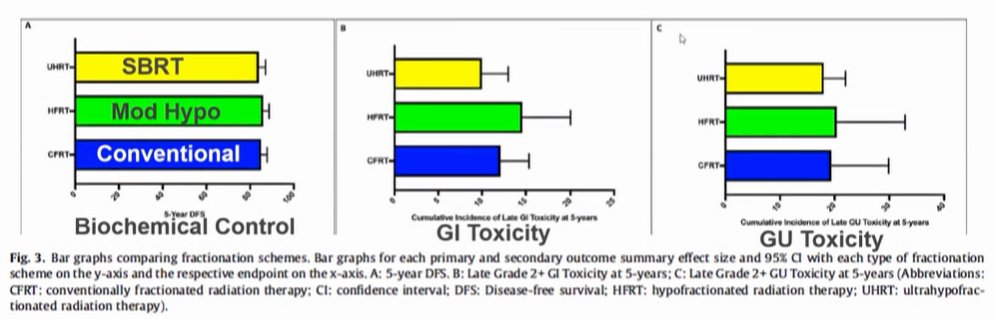
Putting these data together, Dr. Desai argued that biochemical control is comparable with relatively comparable GI and GU toxicity.
Moving forward, Dr. Desai emphasized that a decrease in the number of fractions given may allow for time to improve treatment delivery. One area he highlighted in ongoing work is to assess rectal dose reduction devices, such as hydrogel spacers. Additionally, he highlighted that there remains debate regarding dosing. Previous work has shown that the dominant lesion is the site of most radiotherapy recurrence diseases. Thus, increasing the dose to this region of the prostate may improve biochemical control, without increased toxicity associated with increasing the whole gland dose.
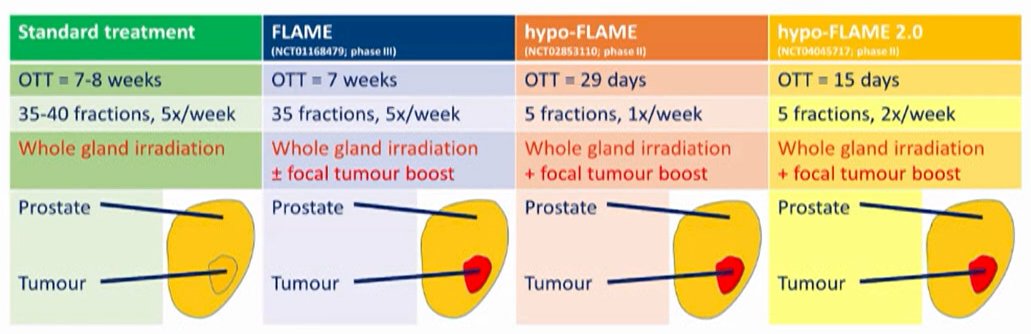
He suggested that this approach is likely the most relevant in patients with high-risk disease. The role of ultra-hypofractionation in patients with high-risk disease has been assessed, to date, in single-arm prospective studies. While there are concerns and challenges regarding the precise alignment of treatment to multiple targets, this approach has received conditional support from the NCCN guidelines panel.
In conclusion, he highlighted that hypofractionation is supported by level 1 evidence for the vast majority of patients, with moderate hypofractionation applicable to all risk groups while ultra-hypofractionation has been assessed predominately in the low-intermediate risk group. Further, moderate hypofractionation can be performed using existing technology while ultra-hypofractionation requires more advanced radiotherapy approaches. Both provide an opportunity to reduce treatment burden and improve the therapeutic ratio.
Presented by: Neil Desai, MD, Radiation Oncology, UT Southwestern Medical Center


