Eligible participants had to report no previous pharmacological treatment for OAB and demonstrate 3 or more episodes of urge urinary incontinence (UUI) on a 3-day voiding diary. Subjects with a predominant stress urinary incontinence were excluded from the study. Once enrolled, participants were asked to return for the PTNM session once a week during consecutive 12 weeks and complete bladder diaries at session 1, 4, 8 and 12. Quality of life questionnaires were administered in clinic during the same time points.
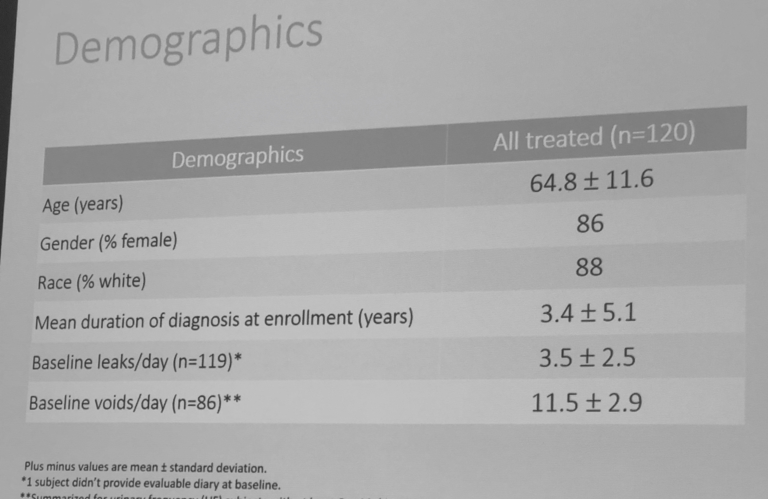
A total number of 154 participants were enrolled into the trial with 116 completing PTNM session 12. Study population was primarily female (86%) with a mean age of 64.8 years and 3.5 baseline leaks (Figure 1).
Data demonstrate a statistically significant decrease in a number of UUI episodes (2.4 episodes at session 12 compared to baseline) (Figure 2). Quality of life measures have statistically improved in the following domains: coping, concern, sleep, social, and symptom bother (Figure 3).
Figure 2:
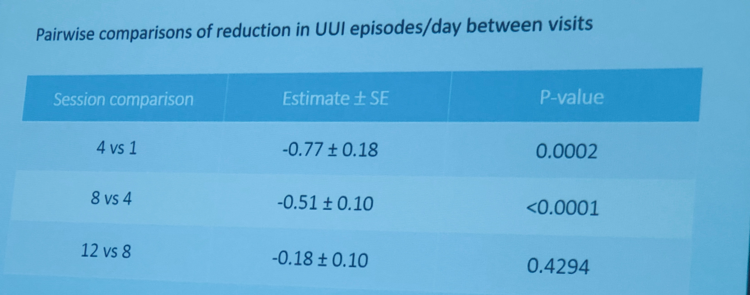
Figure 3:
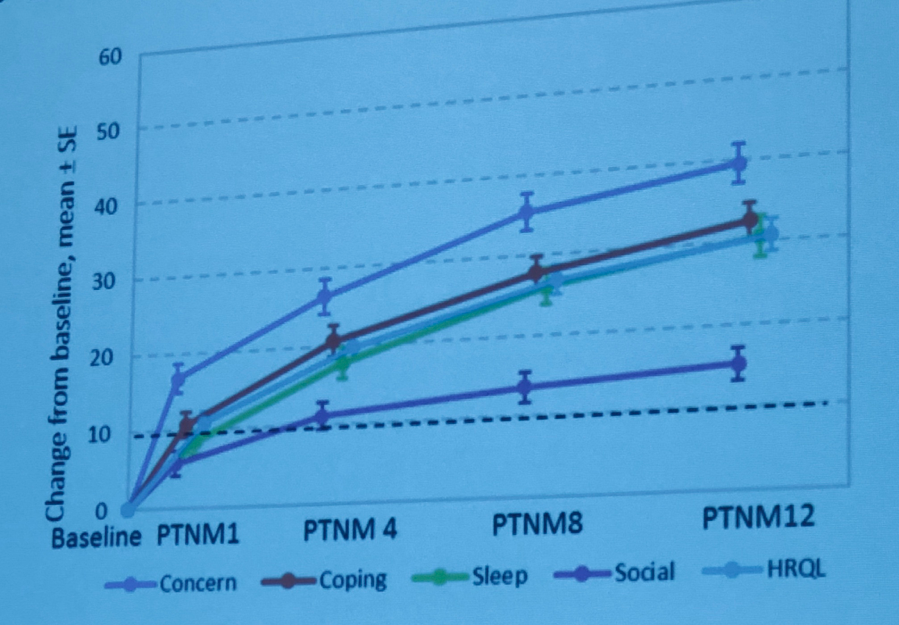
Participants indicated an improvement in the quality of life outcomes related to the OAB, particularly at sessions 4, 8, and 12 (except Social) (all p<0.0001).
The study showed that OAB patients could benefit from PTNM protocol if it’s maintained to up to 12 weeks. It is common for the patients to discontinue their PTNM prescription due to perceived ineffectiveness. This research supports the idea that prolongation and compliance with treatment for more than 6 sessions can positively affect an individual’s quality of life and decrease OAB symptoms. Future research is needed to evaluate if the improvement would last overtime and could lead to the complete dry state.
Presented by: Kathleen Kobashi, MD, FACS, Virginia Mason Medical Center, Seattle, WA
Co-authors: Peter Sand, NorthShore University Health-System, Evanston, IL, Eric Margolis, Urologic Research and Consulting LLC, Englewood, NJ, Steven Siegel, Metro Urology, Woodbury, MN, Salil Khandwala, Advanced Urogynecology of Michigan PC, Dearborn, MI, Diane Newman, Division of Urology, Penn Medicine, University of Pennsylvania, Philadelphia, PA, Victor Nitti, NYU School of Medicine, New York, NY Scott MacDiarmid, Alliance Urology Specialists, Greensboro, NC Anne Miller, Medtronic, Minneapolis, MN, Fangyu Kan, Medtronic, Minneapolis, MN
Written by: Hanna Stambakio, BS, Clinical Research Coordinator, Division of Urology, University of Pennsylvania, Twitter: @AStambakio at the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction Winter Meeting, SUFU 2019, February 26 - March 2, 2019, Miami, Florida


