Scottsdale, Arizona (UroToday.com) Dr. Craig Comiter and team aimed to identify factors associated with no-show and cancellation <24 hours (NCL) in our outpatient urology practice in this retrospective study. Patient satisfaction in an outpatient urology practice (general, andrology, female, neuro-urology, voiding dysfunction) is dependent on efficient clinical workflow to allow patients to be seen in a timely manner.
Patients who do not show up to their appointment, cancel with less than 24-hour notice, or arrive late result in interference in scheduling other patients, loss of physician productivity, and are a source of patient-physician dissatisfaction. Prior research has been in primary care, with a paucity of publications in urology. Some studies have found the benefit of reminders and confirmations, and others no difference. Our aim was to identify factors associated with no-show and cancellation <24 hours (NCL) at Stanford University, of outpatient urology practices.
This was a retrospective analysis of all patient encounters in our outpatient urology clinic from May to December 2018. An encounter dataset was generated by exporting variables directly from the electronic medical record. Using multivariable logistic regression, they identified patient factors associated with NCL versus completed visits. The adjustment was performed for referring service, appointment confirmation method, age, gender, and insurance. Data are presented as odds ratio (OR) with 95% confidence limits.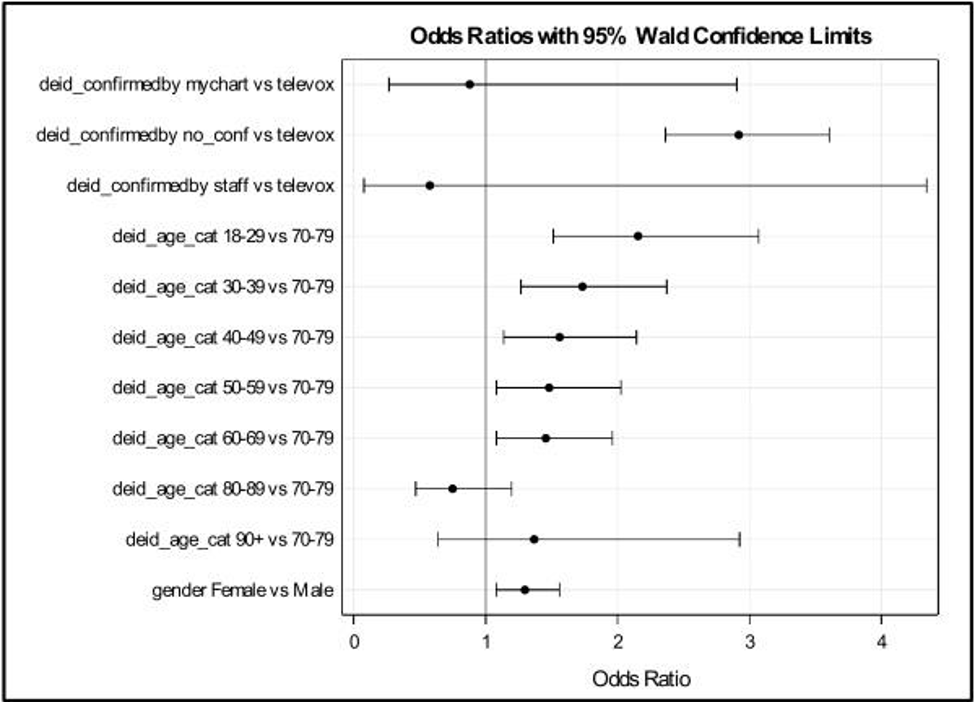
There were 3,428 patients (71.1% male,28.9% female) with a mean age of 56 years (SD=18.2,IQR 40-70) scheduled for 5,431 encounters [1,119 (20.6%) cancellations >24 hours prior to appointment;427 (7.9%) cancellations <24 hours prior to appointment;3,655 (67.3%) completed visits; and 230 (4.2%) no-show]. Among NCL (n=657) versus completed (n=3,655) encounters, appointments were confirmed via: online patient portal (0.5% versus 1.0%); office staff (0.2% versus 0.6%); automated telephone reminder (18% versus 39%); and no confirmation (81.4% versus 59.4%). On multivariable regression, referring service and insurance type were not significantly associated with the outcome NCL versus completed visit. In our final logistic regression model (Figure 1); automated telephone reminder (OR 2.919;95%CI 2.363-3.605),youngest age strata (18-29 years of age OR 2.156;95%CI 1.514-3.070) and female gender (OR 1.298;95%CI 1.080-1.560) were significantly associated with a greater odds of NCL.
Presented by: Amy D. Dobberfuhl, MD, MS, Christina M. Foote, RN, BSN, Norma J. Evaristo, RN, BSN, Angela M. Graf, MS, and Craig V. Comiter, MD
from the Department of Urology at Stanford University


