When cancer patients find out they have a CAT, they undergo a long a complex emotional pathway, called the emotional CAT pathway, described in the PELICAN study, as seen in figure 1.1 They go through different phases with a significant emotional burden.
Figure 1 – Emotional cancer-associated thrombosis pathway – the PELICAN study:
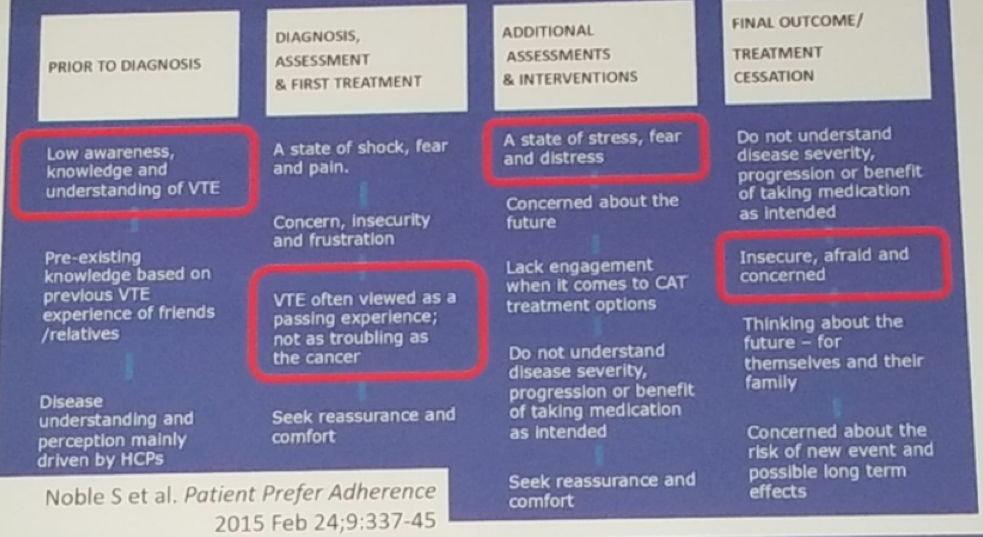
A large portion of cancer patients who have a CAT, are not entirely aware of their increased risk of various dire outcomes, and the practical implications of CAT.2
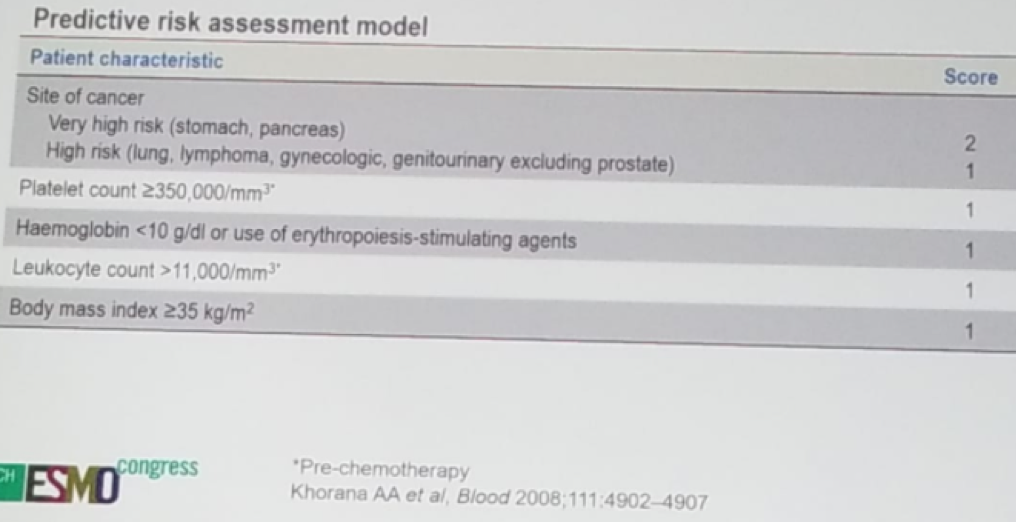
The Khorana score is the most important and only validated risk score for VTE.3 It is comprised of several factors, as can be seen in Table 1. A score of 3 points or more, puts the patient in grave risk for a VTE.
Table 1 – Khorana score for VTE:
There are two ongoing studies that will hopefully answer some questions regarding which cancer patients to treat with anticoagulation. The Cassini study assessed the efficacy and safety of rivaroxaban vs. placebo for VTE prophylaxis in ambulatory cancer patients initiating systemic cancer treatment therapy at high risk of VTE.4 A total of 700 patients were randomized to either placebo or rivaroxaban for a treatment duration of 180 days. The Cassini study has completed recruiting, but no results have been published yet. A similar study is the AVERT study, which compares Apixaban to placebo in the prevention of VTE in high-risk ambulatory cancer patients receiving chemotherapy.5
Current guidelines do not recommend the use of routine thromboprophylaxisin ambulatory cancer patients, other than in high-risk patients. However, every patient should be assessed separately, using the Khorana score. Risk adaptive models that may identify ambulatory cancer patients, who would most benefit from thromboprophylaxisstill need further testing. Evidence for direct oral anticoagulants (DOAC) is lacking, but relevant studies are going to report their results soon.
Low molecular weight heparin (LMWH) is associated with a significant reduction in the risk of recurrent VTE, without a significant increase in major bleeding episodes, when compared to vitamin K antagonists (VKA). The Hokusai-VTE-Cancer study randomized patients with cancer and objectively proven VTE to either LMWH for five days, followed by oral treatment with Edoxaban (an oral anticoagulant drug which acts as a direct factor Xa inhibitor), or to Dalteparin (an LMWH) for 12 months. This was a multicenter study with 114 sites including 1050 patients.6 The primary endpoint was first recurrent VTE or major bleeding event. The study demonstrated that oral edoxaban was noninferior to subcutaneous dalteparin concerning the outcome of recurrent venous thromboembolism or major bleeding. The rate of recurrent venous thromboembolism was lower, but the rate of major bleeding was higher with edoxaban than with dalteparin.
Another study is the SELECT-D study, randomizing patients with active cancer with symptomatic DVT and or any pulmonary embolism, to either Dalteparinor Rivaroxaban (the first available oral active direct factor Xa inhibitor) for 6months with 530 patients randomized.7 The results demonstrated that Rivaroxabanwas associated with relatively low VTE recurrence rate (4% vs. 11%), but higher clinically relevant non-major bleeding compared with dalteparin.
In a systematic review and meta-analysis of these trials, the main conclusion was that DOACs is a feasible option for the treatment of CAT, reducing VTE recurrence. Careful risk assessment of individual clinical circumstances and patient preference need to be considered regarding the bleeding risk.
So how to decide whether the cancer patient should receive DOAC or LMWH or maybe both? Most importantly, this is a shared decision-making process between the patient and the oncologist. It is important to understand what the patient preference is. It is also necessary to consider the burden of cancer and the burden of VTE (LMWH should be considered for patients with severe symptoms). Chemotherapy and other concomitant medications need to be considered as well, and their potential interactions with the anticoagulant given. Renal function, cancer type, nausea and vomiting, and the weight of the patient are all additional important issues to factor in.8
Dr. Young concluded her talk by demonstrating the current updated guidelines regarding anticoagulation treatment in cancer patients. The guidelines recommend individualized treatment regimens after shared decision making with patients. The use of DOACs for cancer patients with an acute diagnosis of VTE, a low risk of bleeding, and no drug-drug interactions with current systemic therapy is recommended. LMWH is always an appropriate alternative. The guidelines recommend using LMWHs for cancer patients with an acute diagnosis of VTE and a high risk of bleeding, including patients with luminal gastrointestinal cancers and patients with genitourinary cancers, or with nephrostomy tubes, who are at an increased risk of bleeding.4
Presented by: Annie Young, MD, University of Warwick, UK
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter: @GoldbergHanan at the 2018 European Society for Medical Oncology Congress (#ESMO18), October 19-23, 2018, Munich Germany
References:
- Noble S et al. Patients’ Experiences of LIving with CANcer-associated thrombosis: the PELICAN study. Patient Prefer Adherence 2015
- Hutchinson A Rees S et al. In press Palliative Medicine
- Khorana AA et al. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008
- Khorana AA et al. Rivaroxaban for Preventing Venous Thromboembolism in High-Risk Ambulatory Patients with Cancer: Rationale and Design of the CASSINI Trial. Rationale and Design of the CASSINI Trial. Thromb Haemost 2017
- Kimpton M et al. Thrombosis Research 2018
- Raskob G et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism NEJM 2018
- Young AM et al. Comparison of an Oral Factor Xa Inhibitor With Low Molecular Weight Heparin in Patients With Cancer With Venous Thromboembolism: Results of a Randomized Trial (SELECT-D). Journal Clinical Oncology 2018
- Reiss H et al. Use of Direct Oral Anticoagulants in Patients with Cancer: Practical Considerations for the Management of Patients with Nausea or Vomiting The Oncologist 2018


