In this single institution, retrospective study, the authors identified 235 patients who were included in an AS program for low-risk PCa, according to the PRIAS criteria (cT1/T2a; PSA<10 ng/ml; PSA density <0.2; Gleason score <7; < 3 positive cores), between 2009 and 2016. Of these 95 men underwent a prostate MRI and were the designated as the study cohort.
Number, size, location and grading (PIRADS score v.2) of mpMRI lesions were recorded. They then compared pathologic outcomes in patients submitted to targeted (fusion and cognitive) biopsies - they correlated mpMRI findings to histopathological results of subsequent biopsies. The rates of clinically significant prostate cancer (csPCa), defined as prostate cancer with Gleason score > 6, was assessed stratified by PIRADS score and biopsy approach (targeted vs. systematic biopsy).
As 18 patients underwent more than one mpMRI, there were 120 mpMRIs for evaluation in the cohort. The median time from protocol entry to mpMRi was 12 months (IQR: 3.75-23.25). In terms of specific mpMRI findings:
- 48 (40.0%) and 72 (60.0%) patients had a PIRADS score ≤2 and ≥3, respectively.
- PIRADS score was 3 in 32 (44.4%), 4 in 31 (43.1%), and 5 in 9 (12.5%) patients, respectively
- Median and mean lesion size at MRI were 9 mm and 9.1 mm (IQR: 6-12)
- 34 (35%) suspicious lesions were localized at the transitional zone of the prostate, while 23 (23.7%), 9 (13.5%), and 27 (27.8%) were found at the apex, the base and the lateral zone of the prostate, respectively
- Eighteen patients (18.9%) had more than 1 suspicious lesion
Suspicious mpMRI led to 75 biopsies, the results of which are summarized below in the table.
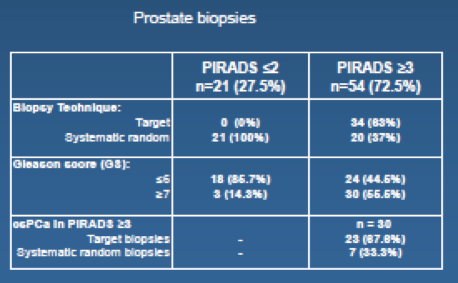
- Of 54 patients with PIRADS ≥3, 30 (55.6%) had Gleason ≥7 on biopsy (any technique)
- Of the 34 that submitted to a targeted biopsy (n=34), Gleason 7 or higher was found in 23 (67.6%) vs. 7 (33.3%) in patients with PIRADS score ≥3 submitted to systematic biopsies (p=0.001)
- However, of patients submitted to targeted biopsy (n=34), Gleason ≥7 outside of the targeted area was found in 7 patients (20.1%)
- Of 21 patients with PIRADS ≤2, 7 (33.3%), 11 (52.3%) and 3 (14.5%) had negative biopsy, Gleason 6 and Gleason 7 or higher at systematic biopsy, respectively
Overall, this resulted in 10 (13%) patients with csPCa that were missed by mpMRI – 3 that were PIRADS ≤2 and 7 that were not in the targeted PIRADS 3+ area.
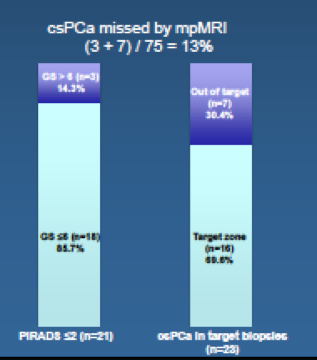
Based on this, the authors conclude that mpMRI should be an important part of AS protocols, as 80% of AS candidates have abnormal mpMRI findings. However, the mpMRI still would have missed 13% of csPCa’s, so it is not yet able to replace biopsies.
Limitations / Discussion Points:
Discussion with the presenter identified that there were many men on AS who received a biopsy and no MRI, for whom results are not available. More importantly, there are men who underwent an MRI but no subsequent biopsy – this data would be important to determine false negative rate of mpMRI.
Based on these findings, the group is changing its practice. mpMRI was ordered on a case by case basis for concerning changes – however, now, they will be switching to a more systematic, scheduled MRI prior to all biopsies.
Speaker(s): S. Lugazzo
Co-Authors: Suardi N., Dell'Oglio P., Cardone G., Gandaglia G., Esposito A., De Cobelli F., Cristel G., Kinzikeeva E., Freschi M., Gaboardi F., Del Maschio A., Montorsi F., Briganti A.
Institution(s):
1. Vita-Salute University San Raffaele, Dept. of Urology, Milan, Italy
2. Vita-Salute University San Raffaele, Dept. of Pathology, Milan, Italy
3. Vita-Salute University San Raffaele, Dept. of Radiology, Milan, Italy
Written By: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto
Twitter: @tchandra_uromd
at the #EAU17 - March 24-28, 2017- London, England


