(UroToday.com) At the 2021 American Urological Association (AUA) Summer School session on the updates in the management of penile cancer, Dr. Philippe Spiess from the Moffitt Cancer Center discussed the management of locally recurrent penile cancer. Dr. Spiess started by highlighting a case presentation of a 56-year-old male presenting with a fungating penile tumor and bulky inguinal nodes. He underwent a partial penectomy consistent with pT2 squamous cell carcinoma (moderately/poorly differentiated) and an ultrasound-guided biopsy of the left inguinal node consistent with squamous cell carcinoma. A metastatic evaluation revealed bulky inguinal nodes bilaterally but no pelvic adenopathy or other distant sites of disease. Dr. Spiess notes that for this patient there are several potential treatment options:
- Upfront surgery: bilateral superficial and deep inguinal lymph node dissection
- Neoadjuvant systemic chemotherapy: followed by inguinal lymph node dissection
- Clinical trial: with no role for surgery
- Palliative/supportive care
The patient refused neoadjuvant systemic chemotherapy so Dr. Spiess proceeded with a bilateral superficial and deep inguinal lymph node dissection with Sartorius myocutaneous flaps and bilateral pelvic lymph node dissection. Pathology demonstrated 3 out of 5 positive superficial inguinal nodes on the right (largest 1.6 cm with extranodal extension present), 1 out of 3 positive superficial inguinal nodes positive on the left (largest 4.0 cm with extranodal extension present), with the deep and pelvic lymph nodes negative bilaterally. The recommendation at this point in time was adjuvant systemic chemotherapy and external beam radiotherapy, and he subsequently received four cycles of systemic TIP, followed by reimaging revealing a single site of suspected disease on PET-CT in the left inguinal area:

At this point in time the patient’s treatment options are as follows:
- Salvage inguinal lymph node dissection (+/- adjuvant therapy/radiotherapy)
- Systemic chemotherapy alone
- Radiotherapy and chemotherapy
- Palliative/supportive care
The patient subsequently underwent a left salvage inguinal lymph node dissection with reconstructive surgery consisting of a rectus myocutaneous flap in collaboration with plastic surgery. To date, the patient has remained without evidence of disease with serial imaging every three to six months, including serial use of PET/CT within the immediate follow-up time period.
Dr. Spiess emphasized that surveillance follow-up should be dictated by the risk of recurrence. As highlighted in a 2008 study from Liejte et al.,1 over 7 years of follow-up the risk of local recurrence continues throughout follow-up necessitating vigilance for local recurrence. With regards to regional recurrence, the curve for recurrence flattens at four years of follow-up, and for distance recurrence at ~18 months of follow-up:

Over the last several years, there has been increased utilization of PET/CT imaging in advanced disease and in the setting of multimodal therapy. Particularly in penile patients with advanced disease, determining which patients should undergo surgical resection following neoadjuvant chemotherapy is unclear. A small study by Graafland et al.2 assessed eight patients who had undergone PET imaging (18F-FDG) at baseline and after two cycles of induction chemotherapy, with metabolic tumor response accurate in all eight patients and 5 of 6 responders continuing chemotherapy, and subsequently undergoing an operation following completion of chemotherapy. Additionally, histopathologic analysis confirmed the metabolic tumor response seen on PET/CT.
Management of locoregional recurrence is also important, with Dr. Spiess highlighting a multicenter (international study across 4 centers) study (including patients from his group at Moffitt) of patients undergoing salvage inguinal resection for penile cancer recurrence following inguinal lymph node dissection.3 Among 20 patients meeting criteria, the meantime to recurrence was 7.7 months. At the time of salvage inguinal lymph node dissection, a median of 3 lymph nodes (range 1 to 17) was resected with a median of 2 (range 1 to 7) nodes positive for malignancy. The median disease-specific survival was 16.4 months, and median overall survival was 10.1 months. Of the initial cohort, nine patients were without evidence of disease, and post-op complications occurred in 11 patients, including wound infections in six patients, postoperative severe (debilitating) lymphedema in four patients, and seroma in one patient.
With advanced disease, Dr. Spiess emphasizes that this often requires extensive reconstruction, of which myocutaneous flaps can be very useful. Specifically, VRAM flaps offer a viable option for large surgical resections with curative or palliative intent. However, patients and the treatment team must be aware and educated regarding the significant risk of complications (upwards of >80%), and continual refinements of these reconstructive techniques and early recognition/vigilance for potential complications cannot be overemphasized.
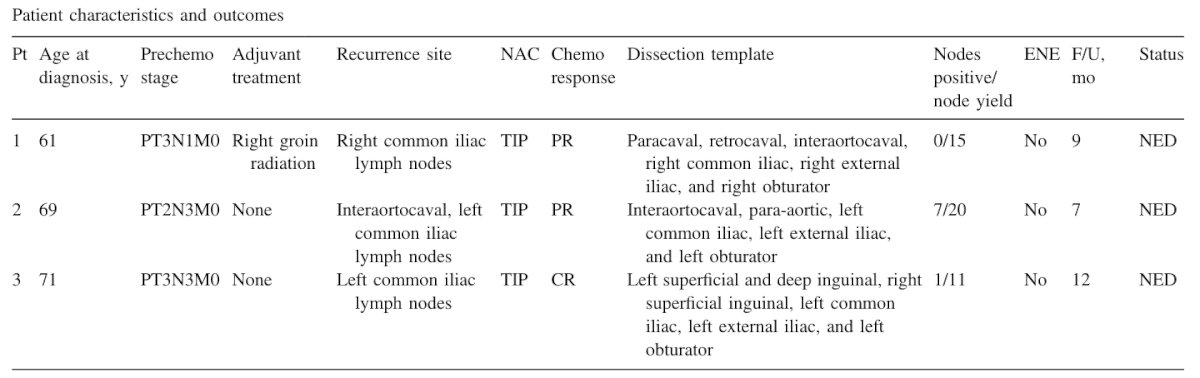
Patients with postchemotherapy lymph node metastases have an inherently poor prognosis and salvage surgery should be highly selective and discussed in a multi-disciplinary setting on a case-by-case basis. As follows is a summary of three patients from Dr. Spiess’ practice that benefited from an aggressive surgical approach:4
Dr. Spiess then discussed recurrent primary tumors, by highlighting penile sparing surgery. In a multi-institutional study of 1,188 patients undergoing penile sparing surgery, Baumgarten et al.5 found that over a median follow-up of 43.0 months there were 252 local recurrences (21.2%), of which 99 (39.3%) developed within the first year. Furthermore, median time to local recurrence was 16.3 months and the 5-year local recurrence-free survival incidence was 73.6%. When stratified by stage, the 5-year local recurrence-free survival rate was 75.0%, 71.4%, and 75.9% in Ta/Tis, T1, and T2 cases, respectively. Only margin status was significantly associated with local recurrence on multivariable analysis (p = 0.001). Among the recurrences noted in this study, the majority were treated with repeat penile sparing surgery.
Salvage surgery may also be needed after radiotherapy to the penis. Dr. Spiess notes that up to 40% of patients who receive radical radiotherapy for penile cancer will eventually need surgery for disease recurrence. Surgery in these patients is often challenging as irradiated tissues are brittle and poorly vascularized making them not ideal for skin grafting. In general, all chronic ulcers or non-healing areas after radiotherapy should be considered tumor recurrence until proven otherwise.
Dr. Spiess concluded his presentation with the following take-home messages:
- Often primary tumor recurrences can be managed with repeat penile sparing treatment approaches, but diligent evaluation and surveillance is critical in doing so
- The effectiveness of current systemic therapies and radiotherapy for advanced/locoregionally recurrent penile cancer remains in question at this time
- If large locally advanced/recurrent tumors are deemed surgically resectable, myocutaneous flaps such as VRAMs are useful realizing they are highly morbid operations even when performed at centers of excellence
- Patients with isolated retroperitoneal recurrences should be considered for multimodal therapy as some are potentially curable, with PET/CT facilitating the evaluation of treatment response
Dr. Spiess concluded with a famous quote from Sir William Osler “The good physician treats the disease; the great physician treats the patient who has the disease.”
Presented by: Philippe E. Spiess, MD, MS, FRCS(C), FACS, Moffitt Cancer Center, Tampa, FL
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the AUA2021 May Kick-off Weekend May 21-23.
References:
- Leijte JAP, Kirrander P, Antonini N, et al. Recurrence patterns of squamous cell carcinoma of the penis: Recommendations for follow-up based on a two-centre analysis of 700 patients. Eur Urol. 2008 Jul;54(1):161-168.
- Graafland NM, Olmos RAV, Teertstra HJ, et al. 18F-FDG PET/CT for monitoring induction chemotherapy in patients with primary inoperable penile carcinoma: First clinical results. Eur J Nucl Med Mol Imaging. 2010 Aug;37(8);1474-1480.
- Baumgarten AS, Alhammali E, Hakky TS, et al. Salvage surgical resection for isolated locally recurrent inguinal lymph node metastasis of penile cancer: International study collaboration. J Urol. 2014 Sep;192(3):760-764.
- Tang DH, Chipollini J, Spiess PE. Postchemotherapy lymph node dissection for isolated retroperitoneal nodal recurrences for penile cancer: Is cure possible in highly selected cases? Urol Oncol. 2018;36:1-3.
- Baumgarten A, Chipollini J, Yan S, et al. Penile sparing surgery for penile cancer; A multicenter international retrospective cohort. J Urol 2018 May;199(5):1233-1237.


