(UroToday.com) The 2023 American Urological Association’s Annual Meeting included a session on Health Services Research: Value of Care, Cost & Outcomes Measures, which featured a presentation by Dr. Daniel Joyce discussing the impact of Medicare subsidies on access, treatment choices, and oncologic outcomes in patients with metastatic prostate cancer (mPCa). The study aimed to explore whether patients who received Medicare Part D low-income subsidies, allowing for reduced out-of-pocket costs for both intravenous and oral cancer therapies, had expanded access and improved outcomes.
Using SEER-Medicare, the authors identified men with advanced prostate cancer aged 66 and older included in the dataset between 2010 and 2017. Using linear probability models, the impact of subsidies on type of initial treatment, oral versus intravenous non-androgen deprivation supplementary systemic therapy was evaluated. Further, the authors estimated overall survival with Kaplan-Meier curves.
The authors identified 5,929 men, of whom, 1,766 (30%) obtained low-income subsidies. In the full cohort, as well as in the subsidy group, oral therapy were the most common supplementary systemic therapy. Upon modeling, men with subsidized care were 17% more likely to receive oral versus intravenous treatments, as compared to men with no subsidy (95% CI 12.1, 22). However, those subsidized men were still less likely to start any supplementary therapy, oral or intravenous, compared to men whose care was not subsidized (probability difference -7.9%, 95% CI -11, -4.8). Low-income subsidy patients experience worse overall survival, as well (p<0.001).
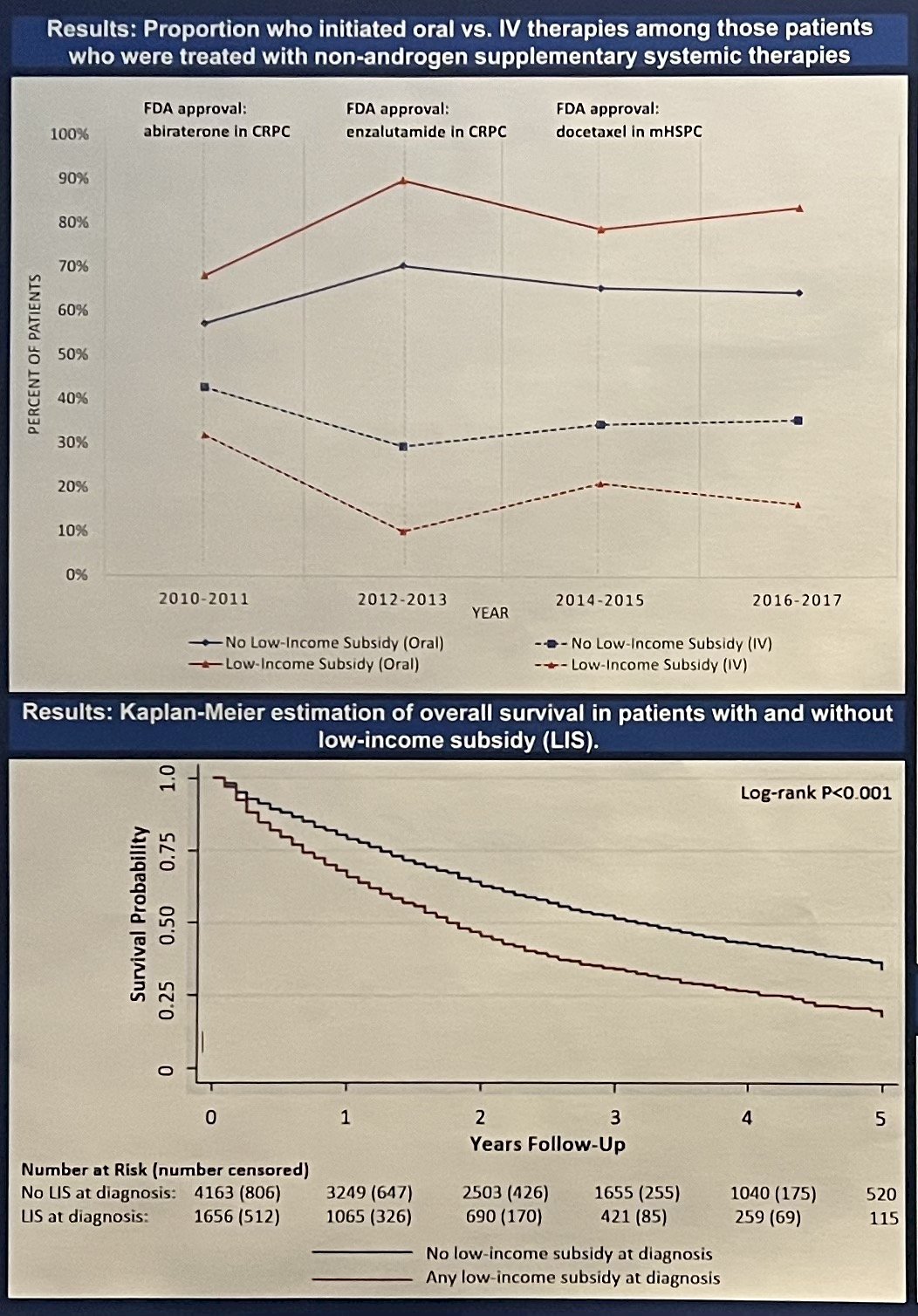
Dr. Joyce discussed that, although subsidies did improve the use of expensive oral therapies in men with metastatic prostate cancer, those men were still less likely to utilize any non-androgen deprivation supplementary systemic therapy. He postulated that this was likely due to additional barriers to access that were not directly addressed by the subsidies. He acknowledged that reduced overall survival was likely a combination of several factors that may or may not have been related to subsidy access, but concluded that a more comprehensive strategy is necessary to improve healthcare access for low-income patients.
Presented by: Daniel Joyce, MD, Mayo Clinic, Rochester, MN
Written by: Ruchika Talwar, MD, Urologic Oncology Fellow, Vanderbilt University Medical Center, during the 2023 American Urological Association (AUA) Annual Meeting, Chicago, IL, April 27 – May 1, 2023


