(UroToday.com) The 2022 ASTRO annual meeting featured a prostate cancer session, including a presentation by Dr. Masatoshi Hotta discussing kinetics and patterns of PSMA PET uptake in prostate cancer after radiation therapy. Radiation therapy is essential in the management of localized and metastatic prostate cancer. Recent studies showed the promising results of PSMA PET guided radiotherapy, particularly in oligometastatic disease. However, the kinetics of PSMA PET uptake in prostate cancer lesions after radiation therapy is unknown. The aim of this study presented by Dr. Hotta and colleagues was to assess the patterns of PSMA PET uptake in irradiated lesions using serial PSMA PET/CT scans.
This was a single-center retrospective study that included patients with prostate cancer who underwent one PSMA PET/CT scan before radiation therapy and at least one other scan after radiation therapy between November 2016 and July 2021. One reader analyzed the target lesions uptake by visual criteria (uptake above background) and semi-quantitative analysis. Lesions with and without residual uptake were compared for:
- Time-interval after radiation therapy
- Lesion tissue type (prostate, prostate bed, lymph node, and bone)
- Radiation therapy type (stereotactic body radiation therapy, intensity-modulated radiation therapy, three-dimensional conformal radiation therapy, and proton therapy)
- Baseline uptake intensity (SUVmax)
- PSMA-derived tumor volume
Lesions with residual uptake were followed-up. Diagnosis of eventual progression was made by biopsy or subsequent follow-up imaging when available.
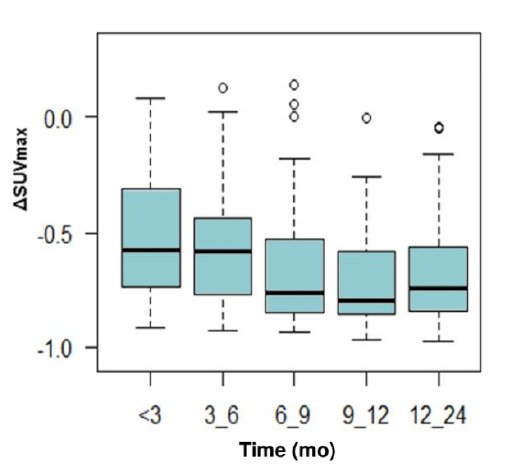
A total of 108 patients with available clinical and imaging data on 257 irradiated lesions (lymph node: n = 126; bone: n = 98; prostate: n = 25; prostate bed: n = 8) were included. The median time from end of radiation therapy to follow-up PET was 10.6 (range: 0.4-51.7) months. Residual uptake after radiation therapy was observed in 90/257 (35.0%) of the irradiated lesions. The mean % decrease in SUVmax of the irradiated lesions on the follow-up PET performed at <3 (n = 20), 3-6 (n = 38), 6-9 (n = 58), and 9-12 (n = 27) months post-radiation therapy were 41.4%, 53.8%, 65.6%, and 69.7% (p = 0.004):
Residual uptake was more commonly seen in the prostate (68.0% vs bone 40.8% vs prostate bed 25.0% vs lymph node 24.8%, p < 0001), and associated with higher baseline uptake and lesion size: SUVmax 9.5 vs 6.4 (p < 0.001) and PSMA-derived tumor volume 1.7 vs 1.0 ml (p = 0.002) in lesions with residual uptake vs. without, respectively. Radiation therapy type was not associated with residual uptake (p = 0.17). In multivariate logistic regression analysis, shorter time after radiation therapy (OR 0.93, 95% CI: 0.89-0.97), higher baseline SUVmax (OR 1.07, 95% CI 1.03-1.11), and lesion in the prostate (OR 6.84, 95% CI 2.19-21.3) were independently associated with residual uptake:
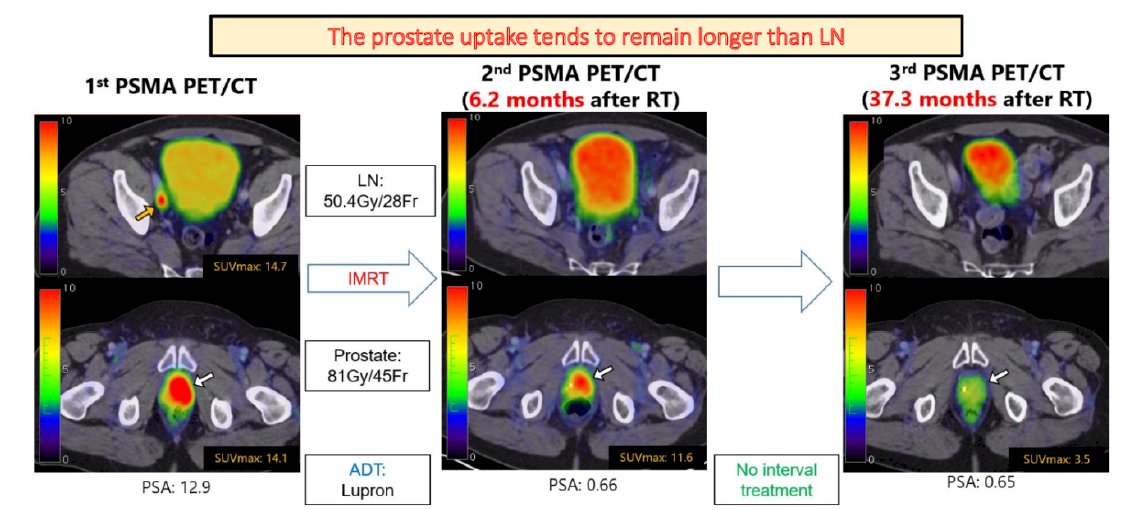
Among the lesions with residual uptake, 28/90 (31.1%) lesions were subsequently evaluated by biopsy and/or follow-up imaging, and 6/28 (21.4%) lesions eventually showed progression. Risk factors of recurrence were a residual uptake observed after a long time-interval from the end of radiation therapy (recurrence vs non-recurrence: 15.8 vs 3.7 months, p = 0.002) in the prostate lesion (prostate 50.0% vs bone 12.5% vs lymph node 0%, p = 0.044). When using a cutoff value of >8.6 months after radiation therapy, the presence of residual uptake was diagnostic of recurrence with a sensitivity of 0.83 and specificity of 0.86 (AUC 0.92, 95% CI 0.81-1.0).
Dr. Hotta concluded his presentation discussing kinetics and patterns of PSMA PET uptake in prostate cancer after radiation therapy with the following concluding messages:
- The PSMA PET uptake of irradiated lesion decreases gradually over one year, reaching its lowest level at 9-12 months
- Uptake in the prostate tends to remain longer than in bone and lymph node lesions
- A longer, persistent uptake (>8.6 months), particularly in the prostate, should suggest a risk of potential local progression
Presented by: Masatoshi Hotta, MD, Ahmanson Translational Theranostics Division, UCLA Nuclear Medicine, Los Angeles, CA
Co-Authors: K. Nguyen1, P. Thin1, W. R. Armstrong1, A. Gafita1, M. Benz1, I. Sonni2, J. Czernin1, N. G. Nickols3, A. U. Kishan4, and J. Calais1; 1Ahmanson Translational Theranostics Division, UCLA Nuclear Medicine, Los Angeles, CA, 2Department of Radiological Sciences, Los Angeles, CA, 3University of California Los Angeles, Department of Radiation Oncology, Los Angeles, CA, 4Department of Radiation Oncology, University of California, Los Angeles, Los Angeles, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Radiation Oncology (ASTRO) Annual Hybrid Meeting, San Antonio, TX, Sat, Oct 22 – Wed, Oct 26, 2022.


