(UroToday.com) The hereditary cancer syndrome Lynch syndrome (LS), molecularly characterized by loss of MLH1, MSH2, MSH6, PMS2) or the EPCAM genes, causes a variety of cancers. Dr. Truong highlights that colorectal and endometrial cancers are the two most common Lynch syndrome-associated cancers with established guidelines for molecular testing. In contrast, upper tract urothelial cancers, (UTUC) a relatively rare cancer, occupies the spot as third most frequent LS-associated cancer, yet the field lacks established guidelines for evaluating UTUC for LS. Identifying this unmet need, the authors sought to propose defined criteria for LS screening selection in UTUC.
To do so, they identified patients with UTUC between April 2015 and April 2021 who received targeted germline sequencing of at least 77 genes associated with cancer susceptibility, with matched normal for comparison. Microsatellites were assessed for instability (MSI) via NGS as well. In addition to sequencing, expression of mismatch repair (MMR) proteins (MSH2, MSH6, MLH1, PMS2 was assessed via immunohistochemical (IHC) staining.

Among the 232 patients with UTUC who received germline testing, median age at the ttme of diagnosis was 67 years (IQR 59-73). A majority (70%) were male. Data on age of diagnosis, histological grade, laterality, and presence of de novo metastasis were summarized in below Table 1.

Germline PGVs (pathogenic/likely pathogentic variants) in moderate- to high-penetrance genes were detected in 31 (13%) patients including 6 (3%) in BRCA1/2 and 21 (9%) in MMR genes (13 MSH2, 4 MSH6, 4 MLH1). A total of 10/21 (48%) patients with MMR PGVs had UTUC as their index cancer. Evaluation of MSI in MMR PGV harboring cases demonstrated 15/16 (94%) with MMR-deficient tumors, with 12/18 with MSI-H.

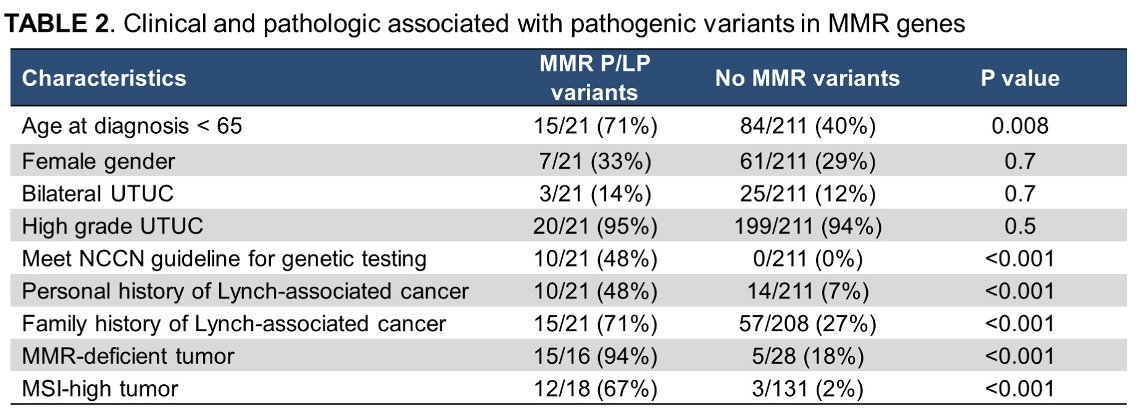
With these data at hand, the authors tested for associations between MMR carrier status and a variety of variables (Table 2). Among these, they demonstrated an association with history (personal and family) of LS core cancers (p < 0.001), age of diagnosis < 65 (p = 0.008), MSI-H status (p < 0.001), and MMR-deficiency (p < 0.001).
No association of MMR PGVs were observed with female gender, high grade disease, or bilateral UTUC. Using established criteria for LS testing (NCCN) displayed high specificity for LS (100%) but did not detect half (11/21) patients with UTUC who harbored MMR PGVs, suggesting in adequacy of existing LS standards.
As the authors conclude, current recommendations for LS referral may be insufficiently sensitive to identify LS-associate UTUC. Given this, the authors recommend UTUC tumors to be assessed for MMR deficiency, MSI, and targeted sequencing both to advise genetic counseling and tailor best systemic treatment options. This presentation will hopefully raise awareness of the need to screen for LS in UTUC patients, and advance the establishment of clear guidelines in the future.
Presented By: Hong Truong, MD MS, Memorial Sloan Kettering Cancer Center, New York, NY
Written By: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Weill Cornell Medicine, and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 17 – Saturday Feb 19, 2022


