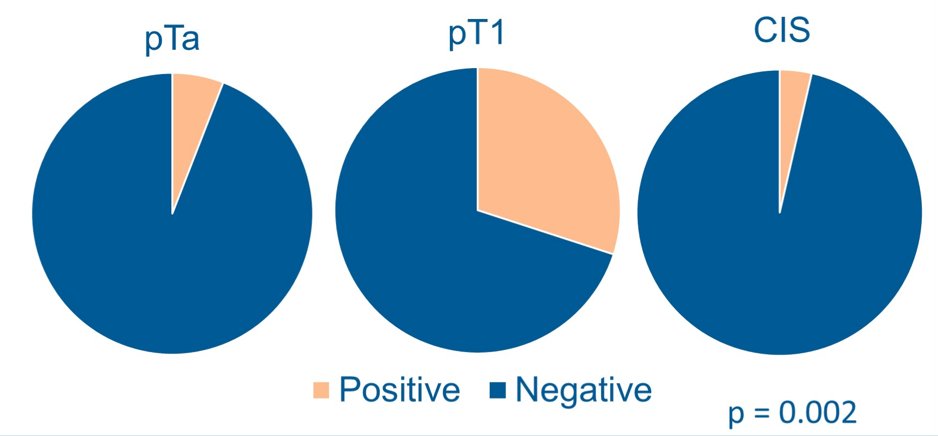
The median follow-up time was 57 months. The median number of BCG maintenance cycles was 1, and 17 (16.7%) patients underwent immediate re-induction BCG. PD-L1 expression was observed 5.9% of pTa, 30.0% of pT1, and 3.6% of CIS (p = 0.002):
BCG unresponsiveness and high grade relapse were observed in 32 (35.6%) and 29 (34.5%) patients, respectively. On univariate analysis, PD-L1 expression was inversely associated with BCG unresponsiveness (OR = 0.112; 95% CI 0.014-0.898) but not high grade relapse (OR = 0.296; 95% CI 0.061-1.440). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of PD-L1 expression for BCG responsiveness were 22%, 97%, 93%, and 41%, respectively:
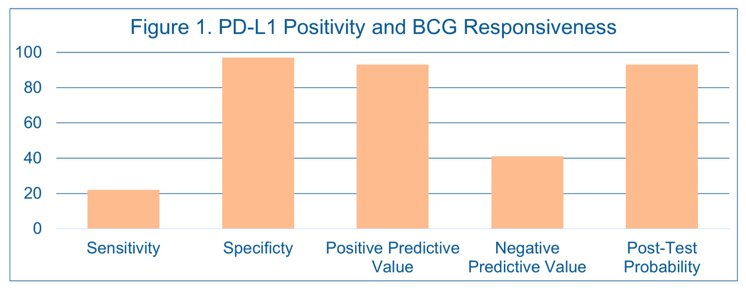
The post-test probability of BCG responsiveness was 93% in patients positive for PD-L1 based on a positive likelihood ratio of 7.33 for PD-L1 expression. On multivariate regression, pT1 (OR 0.159, 95% CI 0.045-0.600), CIS (OR 0.247, 95% CI 0.071-0.857), and PD-L1 expression (OR 15.625, 95% CI 1.779-142.857) were independently associated with BCG responsiveness.
Dr. Woldu concluded his presentation assessing PD-L1 expression and BCG response in NMIBC with the following take-home messages:
- PD-L1 expression in high grade NMIBC was low, and patients with PD-L1 expression at initial TUR were more likely to harbor invasive disease
- Patients showing PD-L1 expression were more likely to demonstrate BCG responsiveness
- These findings suggest a role of PD-L1 in the immune surveillance mechanism of BCG at initial pathologic diagnosis and may assist in predicting responses to BCG among patients with high grade NMIBC
- Further investigation is required to determine if additional immune checkpoint markers have strong correlation with BCG response, particularly among patients without PD-L1 expression
Co-Authors: Thomas Gerald, Vitaly Margulis, Daniel Halstuch, Yaara Ber, Karin Lifshitz, David Margel, Yair Lotan, Liwei Jia
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 17 – Saturday Feb 19, 2022


