(UroToday.com) As the standards of care for advanced urothelial carcinoma (UC) evolve, interpretation of established surrogates for response or prognosis must advance as well. The authors raise the timely question of how the duration of response to immune checkpoint inhibitor (ICI) may be interpretated as prognostic. It was previously been known that a shorter time on first-line therapy or interval between therapies may reflect aggressive disease and portend a worse outcome. The author hypothesize that shorter interval to initiation of second line 2L ICI in advanced UC is associated with worse outcomes.
To test their hypothesis, Dr. Makrakis et al. performed a multi-institutional retrospective cohort study of patients with advanced UC who received platinum-based chemotherapy in the first line, followed by second-line ICI. Maintenance ICI was disallowed. Interval from initiation of first line therapy to second-line ICI was measured, then dichotomized to short (≤6 months) and long (>6 months). Overall response rate (ORR) after ICI initiation, as well as post-ICI progression-free and overall survival were calculated. Analyses were adjusted for Bellmunt risk stratification.
462 of 1283 patients queried received first line platinum-based chemotherapy. Among these 350 (76%) received second line ICI. Cisplatin was the most common platinum used (60%). 270, 269 and 260 patients were eligible and included in analyses of ORR, PFS and OS, respectively. Demographic data included median age of 70 years, a majority male (78%) and white (75%). Histologically 74% were pure urothelial and 21% upper tract.
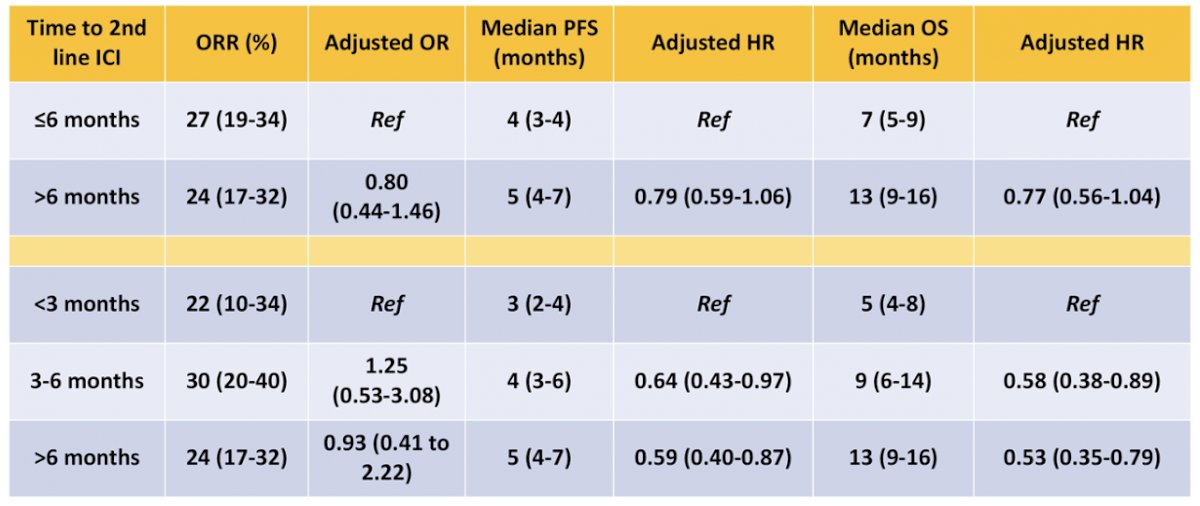
An interval of ≤6 months to initiation of second line ICI was associated with a significantly higher Bellmunt score (2: 32% vs 22; 3: 9% vs 3% score=3). ORR and PFS were comparable between patients with short and long interval to ICI initiation. However, interval of >6 months was associated with significantly longer median OS (13 vs 7 months, p=0.002). A secondary analysis divided further into <3, 3-6, and greater than 6 months, with the group with the shortest interval to initiation of second line ICI as that experiencing shortest PFS and OS.
In conclusion, the authors observe similar ORR and PFS irrespective of short or long interval to initiation of second line ICI following first line platinum chemotherapy, when dichotomized at 6 months. In contrast, OS was more likely to be shorter if time to ICI initiation was ≤6 months. The authors highlight the intrinsic limitations of a retrospective study and confounding biases, without discrediting the value of these data.It remains unclear, but intriguing to consider, that whether these data reflect an impact on disease biology by chemotherapy exposure or intrinsic underlying biology.
Presented By: Dimitrios Makrakis, MD, The University of Washington School of Medicine, Seattle, WA
Written By: Jones Nauseef, MD, PhD, Assistant Professor of Medicine within the Division of Hematology and Medical Oncology, Sandra and Edward Meyer Cancer Center, and Englander Institute for Precision Medicine at Weill Cornell Medicine and Assistant Attending physician at NewYork-Presbyterian Hospital. @DrJonesNauseef on Twitter during the 2022 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, Thursday Feb 17 – Saturday Feb 19, 2022


