(UroToday.com) Immune checkpoint blockade using PD-1 and PD-L1 targeting agents has proven clinical benefit in many metastatic carcinomas. However, identification of patients most likely to benefit has been difficult with most predictive biomarkers examined to date (including PD-1/PD-L1 status and tumor mutational burden) failing to demonstrate clinical utility. CDKN2A is one of the most commonly altered genes across human cancers and offers the potential as a predictive biomarker. However, currently available data are conflicting with respect to the association between CDKN2A alterations and ICBs. Thus, in a poster presentation at the 2021 American Society of Clinical Oncology Genitourinary Cancers Symposium (ASCO GU), Dr. Nassar and colleagues examine the effect of CDKN2A alterations on clinical outcomes in patients with urothelial carcinoma received immune checkpoint blockade (ICB).
To do so, the authors examined a cohort of 809 patients at the Dana Farber Cancer Institute (DFCI) who received treatment with ICBs only and who had relevant cancer types and targeted exome sequencing data (Oncopanel) available. Among these 809 patients, 235 (29%) had loss-of-function (LOF) mutations or homozygous deletions in CDKN2A. The authors compared overall survival between CDKN2A altered and CDKN2A wild type (WT) patients using Cox models while accounting for prior lines of therapy and tumor mutational burden (TMB). The authors further validated their results in a similar cohort from Memorial Sloan Kettering Cancer Center (MSKCC; n=811). Finally, as a control, the association between CDKN2A alterations and overall survival (OS) was examined in a cohort of platinum-treated UC patients (N = 56).
The authors first examined the prevalence of CDKN2A alterations in the Dana Farber Cancer Institute (DFCI) and Memorial Sloan Kettering Cancer Center (MSKCC) cohorts. Such alterations were found in 32/90 (35%) and 22/104 (21.2%) of patients with urothelial carcinoma, from DFCI and MSKCC, respectively; 4/55 (7.3%) and 3/131 (2.3%) of patients with renal cell carcinoma, respectively; 73/178 (41%) and 45/194 (23.2%) of patients with melanoma, respectively; 86/370 (23.2%) and 26/260 (10%) of patients with non-small cell lung cancer (NSCLC), respectively; 18/66 (27.2%) and 4/53 (7.5%) of patients with esophagogastric tumors, respectively; and 22/50 (44%) and 11/69 (15.9%) of patients with head and neck tumors, respectively. Over a median follow-up of 27 months in the DFCI and 24 months in the MSKCC cohorts, CDKN2A alterations were associated with shorter OS and TTF in the DFCI UC and melanoma cohorts by after multivariable adjustment. Further, CDKN2A alterations showed a trend towards significance in the MSKCC UC cohort. 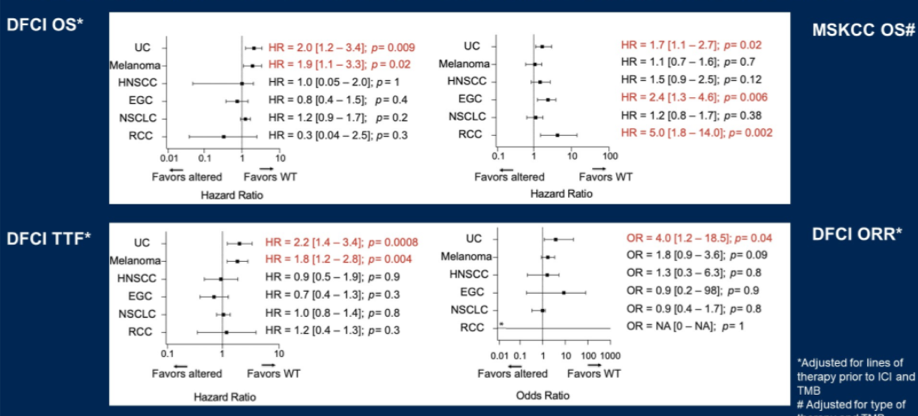
However, in other tumor types, there was no significant association between CDKN2A alterations and OS. Further, in patients with cisplatin-treated urothelial carcinoma, there was no association between CDKN2A alterations and OS. 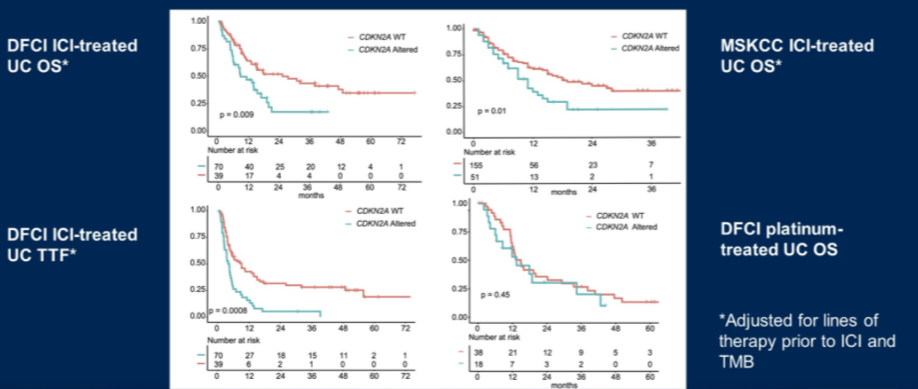
Thus, the authors conclude that CDKN2A alteration status may serve as a unique predictive biomarker in patients with urothelial carcinoma undergoing treatment with immunotherapy. However, these results require further validation and mechanistic study.
Presented by: Amin Nassar, MD, post-doctoral research fellow at the Lank Center for Genitourinary Oncology, Dana-Farber Cancer Institute, Brigham and Women's Hospital
Co-Authors: Elio Adib, Elie W. Akl, Sarah Abou Alaiwi, Pier Vitale Nuzzo, Tarek H. Mouhieddine, Guru Sonpavde, Robert I. Haddad, Marios Giannakis, F. Stephen Hodi, Toni K. Choueiri, David J. Kwiatkowski
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter during the 2021 American Society of Clinical Oncology Genitourinary Cancers Symposium (#GU21), February 11th-February 13th, 2021


