(UroToday.com) The 2022 Advanced Prostate Cancer Consensus Conference (APCCC) Hybrid Meeting included a session on the management of metastatic hormone sensitive prostate cancer (mHSPC) and a presentation by Dr. Ian Davis discussing that when low-volume disease on conventional imaging becomes high-volume on next-generation imaging in mHSPC, we should treat these patients like high volume patients.
Dr. Davis notes that ‘treating like high volume’ means that we should offer patients triplet ADT + androgen receptor inhibitor + docetaxel, given that in ARASENS1 86% of patients had synchronous M1 disease (all deemed to require docetaxel), and in PEACE-12 100% of patients had M1 disease (with an OS benefit so far for high volume disease). At the very least, patients should be receiving doublet therapy. Patients should not be offered ADT alone, and we know that we should not be doing this for patients with low-volume disease anyway, based on data from STAMPEDE, LATITUDE, ARCHES, ENZAMET, TITAN, PEACE-1, and ARASENS. With regards to radiation to the primary tumor, this is the subgroup of the low-volume group that is least likely to receive a survival benefit from radiation to the primary.
Dr. Davis notes that low-volume disease on conventional imaging becoming high-volume on next-generation imaging is stage migration (the “Will Rogers” phenomenon), but he argues that it does not matter given that we should be providing personalized, risk adapted therapy anyway, and that we are using the best imaging tools available. Of note, before next-generation imaging these patients were previously in the “low volume cohort” but were truly in the “high volume cohort” and thus had lower burden of disease than other patients with high-volume disease. This previously worsened the prognosis for the low-volume group but is now improving the prognosis for the high-volume group.
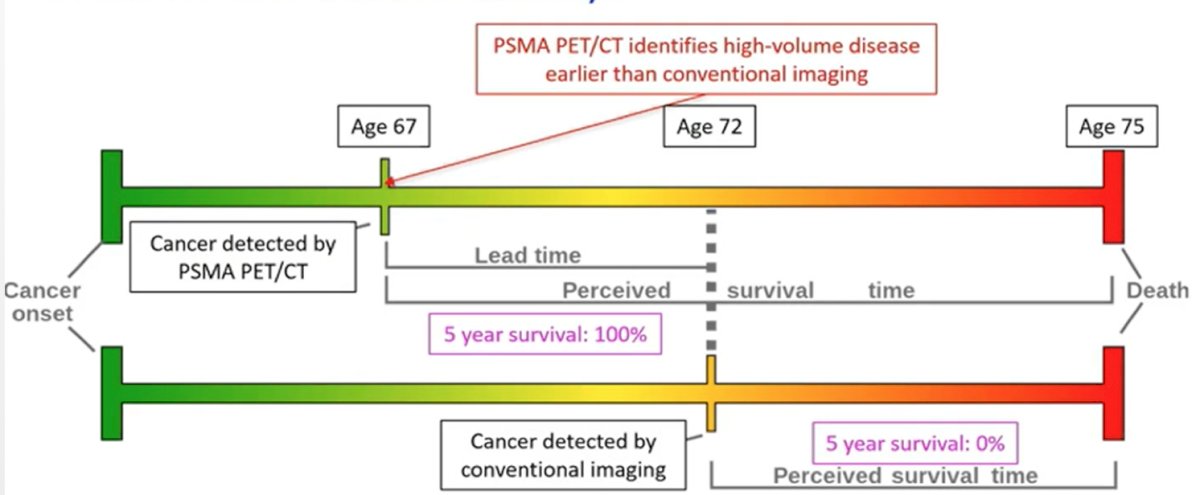
Dr. Davis also emphasized that lead time bias does not matter if treatment will be needed anyway, as highlighted in the following figure:
Dr. Davis then discussed Pascal’s Wager, which states that “a rational person should live as though God exists and seek to believe in God.” If God does not exist, then not much is lost and you’ve been a decent human, however, if God exists, then there are infinite gains in heaven while avoiding hell. Applying this analogy to high-volume mHSPC, if treatment of high-volume disease does not matter, we possibly over treat a few patients with triplet therapy, otherwise, there are unlikely to be detrimental outcomes. Patients probably would need this treatment eventually, and it is just being given earlier than strictly necessary. If treatment of high-volume disease is important, it maximizes the probability of benefit with less chance of inherent resistance, maximizing the probability that treatment will actually be given (better tolerability), and avoids the harm of not treating patients when they should have been treated.
Dr. Davis concluded his presentation of treating patients like high-volume disease when conventional imaging shows low volume disease and next-generation shows high volume disease among men with mHSPC with the following take-home messages:
- Modern imaging is here to stay
- Stage migration is not applicable if we are actually defining a different disease state. The caveat is that we do not know if the same rules apply for metachronous as for synchronous disease
- We can now better select for treatment: (i) those that are most likely to benefit from therapy we should target for more effective therapy, and (ii) those that are least likely to benefit from therapy we should spare from unnecessary intensification and maybe even de-intensify treatment
- Lead time bias does not matter if treatment will be needed anyway
- Pascal’s Wager suggests that a rational person would treat patients as high-volume disease
Presented by: Ian Davis, MD, PhD, Monash University and Eastern Health, Chair of the ANZUP Cancer Trials Group, Melbourne, Australia
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 Advanced Prostate Cancer Consensus Conference (APCCC) Annual Hybrid Meeting, Lugano, Switzerland, Thurs, Apr 28 – Sat, Apr 30, 2022.
References:- Smith MR, Hussain M, Saad F, et al. Darolutamide and Survival in Metastatic, Hormone-Sensitive Prostate Cancer. N Engl J Med. 2022 Mar 24;386(12):1132-1142.
- Attard G, Murphy L, Clarke NW, et al. Abiraterone acetate and prednisolone with or without enzalutamide for high-risk non-metastatic prostate cancer: A meta-analysis of primary results from two randomized controlled phase 3 trials of the STAMPEDE platform protocol. Lancet 2022 Jan 29;399(10323):447-460.


