To avoid unnecessary biopsies, it is important that we use risk calculators, and use serum and urine-based biomarker tests. Dr.Jun Hyuk Hong believes that there is a significant role for mpMRI before first prostate biopsy, and this is a tremendous tool, enabling us to diagnose clinically significant disease in a more accurate way. mpMRI will help predict cancer location, and specifically of clinically significant cancer. It can also assist in the reduction of over-detection of low risk tumors. Another important point which is not often discussed, is that mpMRI can also assist in overcoming post-biopsy changes such as hemorrhage and inflammation.
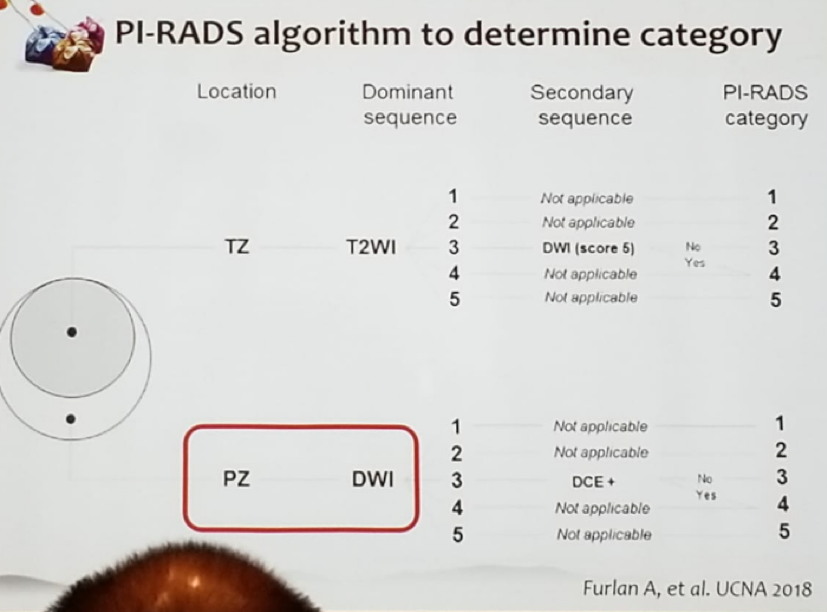
The PIRADS scoring system used to score a prostate lesion identified on mpMRI is from 1 to 5. The chances of a PIRADS 1 lesion harboring any cancer and clinically significant cancer are 25% and 0%, respectively. However, for a PIRADS 5 lesion, the chances of it harboring any cancer and clinically significant cancer are 87% and 72%, respectively. 2 Dr. Jun Hyuk Hong gave a simplified algorithm for the use of the PIRADS scoring system in mpMRI, specifying which phase of the four phases in mpMRI (T1, T2, DWI, and DCE) we need to use for lesions located on the peripheral and transitional zones (Figure 1).
Figure 1 – PIRAD algorithm in mpMRI to determine category of lesion:
mpMRI has been demonstrated to decrease the rate of detection of low risk prostate cancer. Microfocal tumor was detected in 20-25% of patients who underwent systematic standard biopsy, while it was detected in only 0-9% of patients who underwent an mpMRI targeted biopsy.3 The PROMIS study compared the diagnostic accuracy of mpMRI to that of transrectal ultrasound (TRUS) biopsy (with the reference being templated mapping biopsy). This study demonstrated that for clinically significant prostate cancer, mpMRI was more sensitive than TRUS biopsy (93% vs. 48%). The PROMIS study also showed that using mpMRI may allow 27% of patients to avoid unnecessary biopsies and diagnose 5% less insignificant cancer.4 The more recent PRECISION study, published in the New England Journal of Medicine in 2018 5 randomized and compared biopsy naïve men to either standard systematic TRUS biopsy or mpMRI targeted biopsy. The results were very clear, demonstrating that mpMRI targeted biopsy diagnosed 12% more clinically significant cancer (38% vs. 26%) and 13% less insignificant cancer (9% vs 22%), with a higher percentage of cancer per core (44% vs. 18%).
Before concluding his talk, Dr. Jun Hyuk Hong discussed a phenomenon that is important to recognize. This is the post-biopsy hemorrhage, which is a real problem, as it is seen in 49% of patients 3 weeks following a biopsy, lasting up to 4 months. In mpMRI in T2 phase there is decreased signal, which can mimic or obscure an area of a tumor. In T1 phase the hemorrhage will cause a focal or diffuse high signal. The prostate secretes citrate which has an anticoagulant effect. However, prostate cancer causes a significant reduction of citrate secretion, which leads to less hemorrhage in the areas of cancer, producing an “hemorrhage exclusion sign”. It is important to look at the T2 an T1 phase to recognize this, and the tumor hiding behind it.
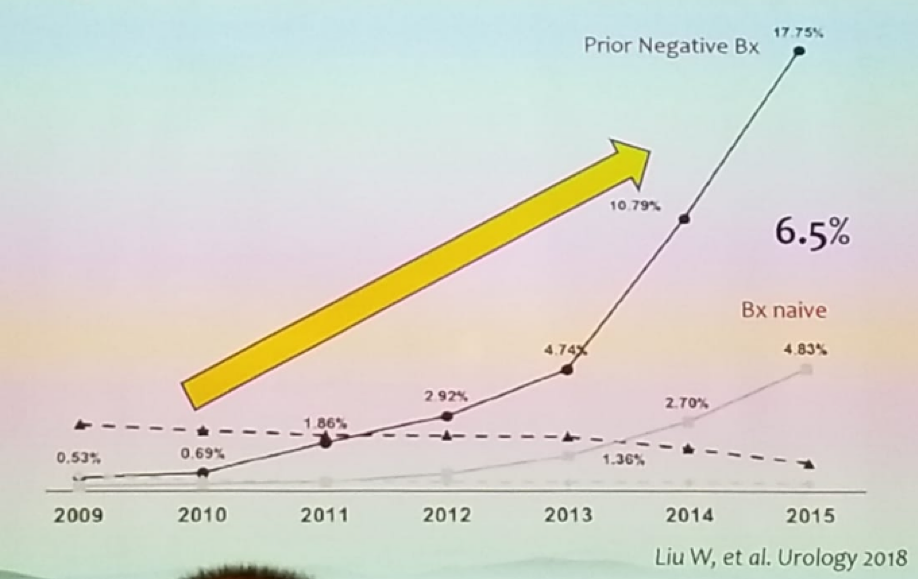
A major hurdle to the use of mpMRI is its cost. In many countries worldwide, mpMRI can be reimbursed only after the diagnosis of cancer. In Korea, “out-of-pocket” cost of an mpMRI before prostate cancer diagnosis is more than 1100 USD, while after diagnosis it is only 20 USD. This significant difference in cost is seen in other countries in the world as well. There is data demonstrating that mpMRI targeted biopsy has a higher detection rate of clinically significant cancer in men with a previous negative biopsy as opposed to men who are biopsy naïve.6 However, the use of pre-biopsy mpMRI in the US has been significantly rising in the last years, together with the use of mpMRI in the setting of prior negative biopsy, as can be seen in figure 2.
Figure 2 – The use of mpMRI in biopsy naïve patients and in patients with prior negative biopsy in the US:
The current European Association of Urology (EAU) guidelines recommend usage of mpMRI only in the setting of prior negative biopsy, when clinical suspicion of prostate cancer persists, despite the previous negative biopsy (level of evidence 1a). The guidelines also state that systematic biopsy should always be performed in addition to mpMRI targeted biopsy.
In summary, Dr. Jun Hyuk Hong believes that mpMRI is the primary imaging modality in the diagnosis pathway of prostate cancer. It may improve the detection rate of clinically significant prostate cancer and reduce the detection rate of clinically insignificant cancer. It is especially useful for anteriorly located tumors, and despite being controversial, and the lacking level one evidence, Dr. Jun Hyuk Hong believes mpMRI should be performed in all patients prior to a biopsy.
Presented By: Jun Hyuk Hong, Asan Medical Center South Korea
References:
- Thompson IM, et al, NEJM 2004
- Mehralivand S. et al. J Urol 2017
- Delongchamps NB et al. J Urol 2013
- Ahmed HU, et al. Lancet 2017
- Kasivisvanathan V et al. NEJM 2018
- Schoots IG et al. Eur Urol 2015


