To address this question, the authors conducted a retrospective study using an international (Europe, USA, UK, Brazil, and China) that contained adequate clinical information on 504 patients who underwent inguinal lymph node dissection. Of these patients, 44.6% received perioperative chemotherapy, and 9.7% received peri-operative radiotherapy.
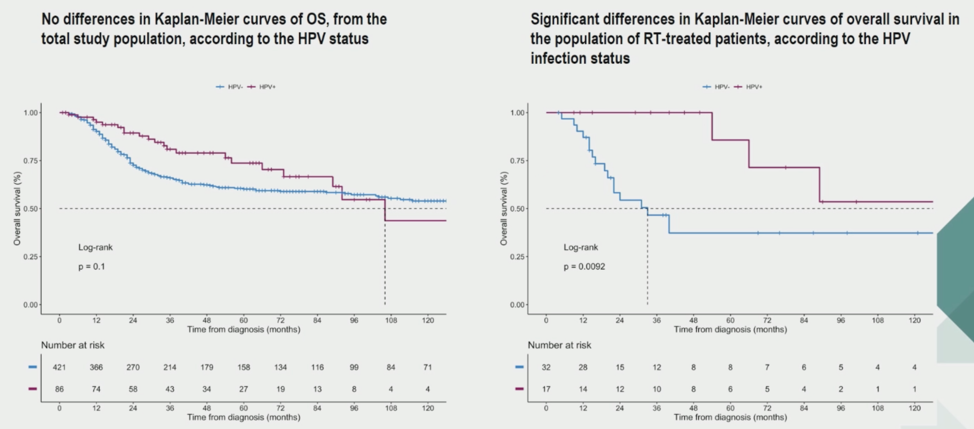
HPV status was not associated with overall survival in this cohort but was associated with improved overall survival in patients who received peri-operative radiotherapy. These findings were consistent when the authors adjusted for prognostic factors like age, histology, surgery, pT2 tumor, nodal stage, and others.
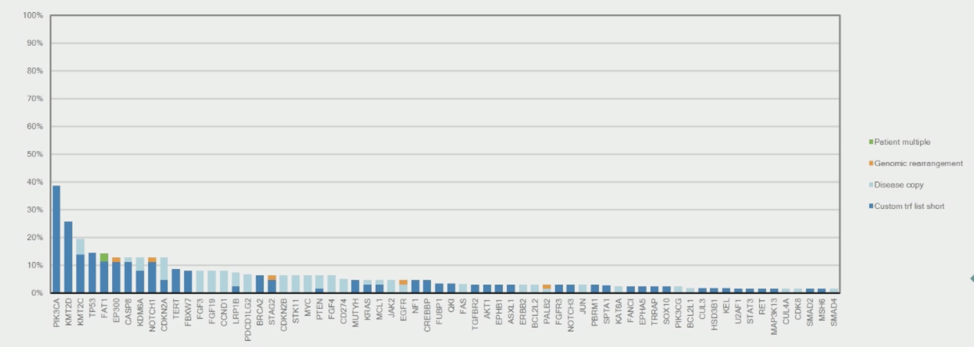
The authors then utilized genomic data from 199 patients whose tumors were sequenced by Foundation Medicine, including 62 that were HPV-positive. Only 1 patient tumor was MSI-H. Within HPV positive patients only 1 tumor was MSI-H. The median TMB was 5.2 muts/mb, with 27% of cases having a TMB > 10 muts/mb and 13% of cases having a TMB > 20 muts/mb. The most common genomic alterations were in the PIK3CA gene, with the rest shown below.
Within HPV-negative patients, one tumor was MSI-H. The median TMB was 3.2 muts/mb, with 10% having TMB > 10 muts/mb and 2% with TMB > 20 muts/mb. The most common alterations in HPV-negative penile cancers were in TP53.
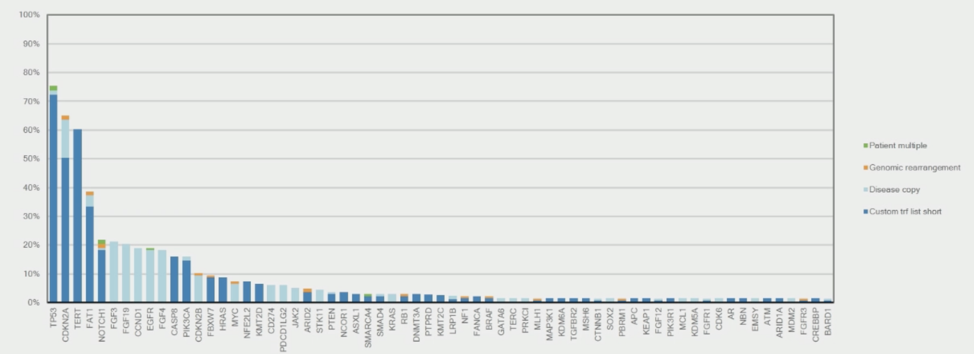
In summary, this study identified lower rates of TP53 alterations in HPV-positive penile cancers, perhaps contributing to their relative radiosensitivity, and identified higher rates of PIK3CA mutation in these tumors.
Presented by: Andrea Necchi, MD, Medical Oncologist, Department of Medical Oncology, Fondazione IRCCS - Istituto Nazionale dei Tumori, Milan, Italy
Written by: Alok Tewari, MD, PhD, Medical Oncologist at the Dana-Farber Cancer Institute, at the 2020 European Society for Medical Oncology Virtual Congress (#ESMO20), September 19th-September 21st, 2020.


