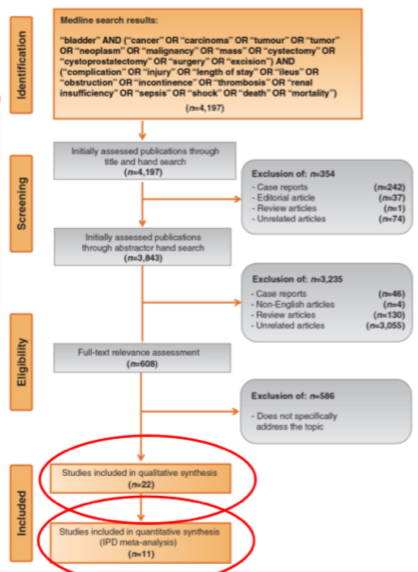
The authors performed a systematic review using Ovid and Medline platforms to identify all relevant articles published from 1970 through 2018. Among identified relevant papers, the authors requested individual patient data (IPD) for meta-analysis.
The authors' literature search identified 4,197 articles of which 22 (0.5%) studies, reporting 3,847 patients, were selected for review.
Of the 18 observational studies which met inclusion criteria, length of stay followed by 30 and 90-d complications were the most studied primary endpoints following the implementation of ERAS protocols. Only a single study in radical cystectomy patients to date has assessed the impact of all 26 ERAS items on outcomes following radical cystectomy.
On the basis of aggregate data reported, ERAS use was associated with reduced morbidity, quicker bowel recovery, and shorter LOS with no increased risk of mortality.
Of the 18 studies which met inclusion criteria, IPD was obtained for 11 studies from 6 centers reporting 2,077 patients. In multivariate analysis, ERAS factors associated with an increased LOS included the use of bowel preparation (Odds Ratio (OR): 5.11; 95% Confidence Interval (CI), 2.18-11.97, p<0.001), and use of a nasogastric tube (NGT) postoperatively (OR: 3.19; 1.45-7.03, p=0.004), while the use of rectus sheath/local anesthesia blocks vs. spinal/epidural was associated with a shorter hospital stay (OR: 0.56; 0.35-0.91, p=0.020).
The authors concluded that, among patients undergoing radical cystectomy, implementation of ERAS protocols was associated with reduced LOS and postoperative complication rates with no increased risk of mortality. Particularly relevant factors associated with decreased hospital length of stay included the elimination of bowel preparation and the use of post-operative NGT, and the use of regional anesthesia.
Presented by: Stephen Williams, MD, MS, FACS, Chief, Division of Urology, Associate Professor, The University of Texas Medical Branch at Galveston, Galveston, TX, USA
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Nashville, TN, USA, Twitter: @WallisCJD, at the 2020 American Urological Association (AUA) Annual Meeting, Virtual Experience #AUA20, June 27- 28, 2020.


