Novel imaging modalities or modifications to current imaging modalities that can help distinguish benign from malignant are being evaluated. In this study, the authors assess CT-based shape and texture as an assessment to discriminate between malignant and benign lesions. Additional imaging metrics (e.g. tumor shape and texture) have been shown to improve discrimination. Using a computer algorithm to quantitatively analyze shape and texture features of renal tumors in three dimensions on routine imaging, the authors created an objective non-invasive method to evaluate tumor behavior. They then tested these “radiomics” framework in objectively distinguishing between benign and malignant renal masses on imaging. They then also determined whether shape shows independency from texture in discriminating benign from malignant masses.
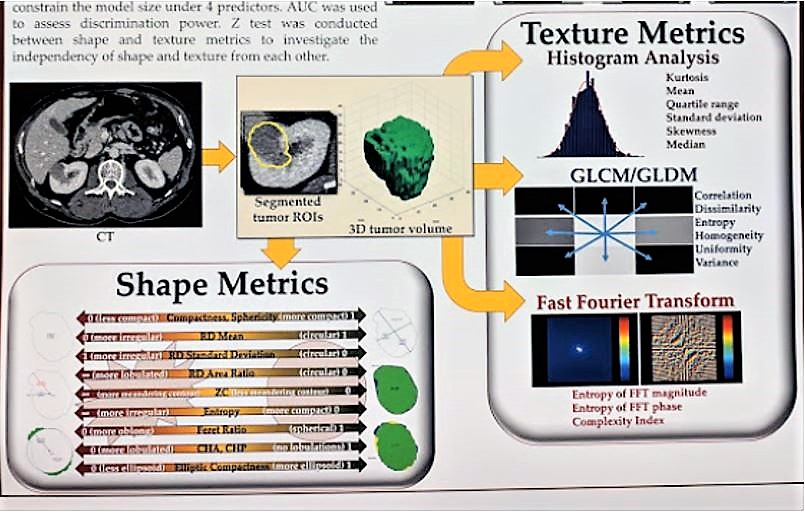
Multiphase computed tomography (CT) images of 135 patients with 94 malignant and 41 benign masses diagnosed between 2011 and 2014 were segmented. Point coordinates of tumor contours in all axial slices were input into a MATLAB (MathWorks) algorithm – this enabled the shape and texture metrics: 33 shape metrics and 760 texture metrics were calculated per tumor. They then used least absolute shrinkage and selection operator (LASSO) to nominate important shape and texture metrics respectively in discriminating benign and malignant masses and then used lambda value to constrain the model size under 4 predictors. The area under the curve (AUC) was used to assess discrimination power to identify the best predictors.
This workflow is seen below:
Based on the above analysis, they identified “sagittal elliptic compactness” and “coronal Feret ratio” as the best shape metrics, and “minimal signal” and “entropy in corticomedullary and excretory phases” respectively as the best texture metrics. AUC using both shape and texture (0.88) was significantly greater than the AUCs using only shape (0.64) and texture (0.82) alone (p = 0.05). This can be seen in the figure below. Moreover, there was a statistically significant difference between AUCs for shape metrics and texture metrics (p = 0.01).
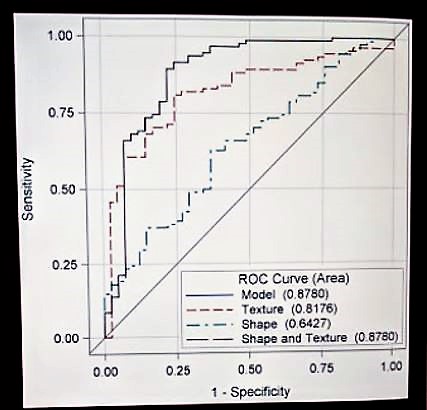
Based on these results, they conclude that shape is an independent predictor in distinguishing benign from malignant tumors, but in order to distinguish benign from malignant renal masses, combining both shape and texture metrics in a single radiomics panel outperforms shape and texture metrics in isolation from each other.
Future studies will determine further clinical applications of their evolving radiomics panel and its potential for better understanding of natural history, behavior, and growth of renal tumors.
Presented by: Felix Y. Yap, MD, Body Imaging & Intervention Fellow, Keck School of Medicine, University of Southern California, Los Angeles, California
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, @tchandra_uromd, @JEFFUrology at American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


