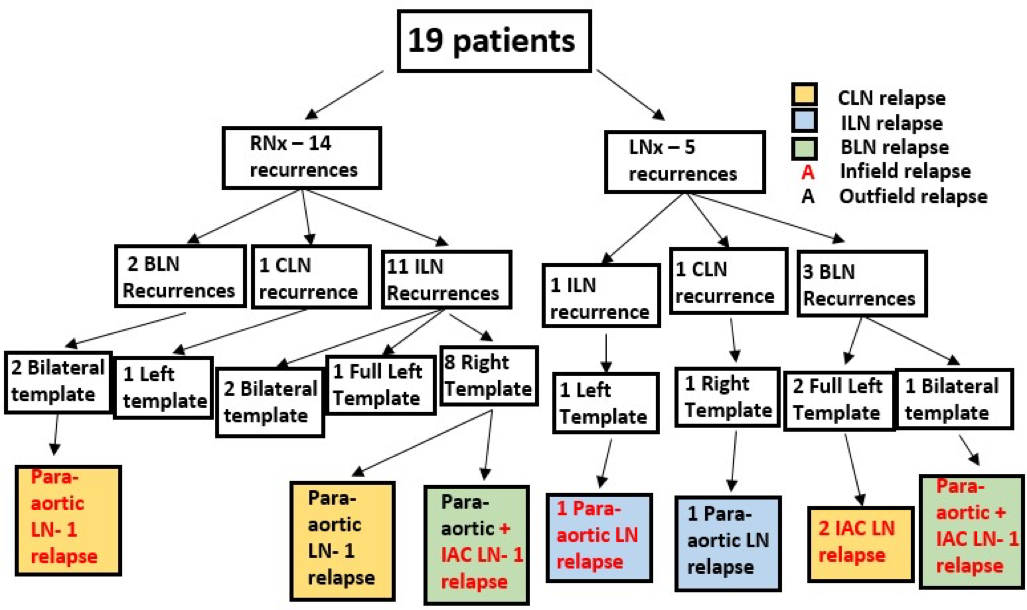
Dr. Barboza then summarized the methodology. This was a retrospective study of 19 patients undergoing RPLND for RCC recurrences between 2011 and 2018. All patients included initially had primary non-metastatic RCC, and subsequent recurrence restricted to the retroperitoneal lymph nodes (LN). The initial LN recurrence site was defined relative to the side of nephrectomy (ipsilateral (ILN), contralateral (CLN), or bilateral (BLN)). The RPLND templates were either full bilateral, right modified, left modified, or a full left (Interaortocaval (IAC) +Para-aortic(PA) LNs). LN relapses after RPLND was assessed.
Dr. Barboza then presented the results of this study. The median age was 60 years at RPLND. Median follow-up after RPLND was 29 months (IQR 22-38). The median time to recurrence after the initial nephrectomy was 10 months. Right or left nephrectomies were performed in 14 (73.7%) and 5 (26.3%), respectively. The extent of lymphadenectomy during nephrectomy varied based on the surgical approach. After right nephrectomy, there were 2 BLN, 1 CLN, and 11 ILN recurrences, while after left nephrectomy, 3 BLN, 1 CLN, and 1 ILN recurrences. These recurrences were treated according to the surgeon’s preference. After RPLND, 8 patients relapsed in the retroperitoneum, 5(62.5%) infield only (2 PA, 1 PA+IAC, 2 IAC), 2(25%) out-of-field only (2 PA) and 1(12.5%) in/out-of-field (in-IAC/out-PA). Only 3 patients relapsed outside the RPLND template, 2 of 8 (25%) after a right template for right nephrectomy ILN recurrence, and one patient after a right template for left nephrectomy CLN recurrence. Eight (42%) patients remained disease free during the follow-up.
Based on the results of this study, Dr. Barboza then concluded that overall the chance of infield relapse in IAC and PA LNs is high due to the local aggressiveness of LN metastasis and/or a lack of standardized LN dissection at initial nephrectomy. Regardless, if RP recurrence occurs, a full bilateral standardized RPLND should be considered. Furthermore, RPLND can achieve complete remission in a significant proportion of RCC patients with a node only recurrences.
During the discussion after this presentation, there was a consensus that prospective studies should be performed to identify patients who will benefit from RPLND in this setting.
Presented by: Marcelo Barboza, MD, Indiana University, Indianapolis, Indiana
Written by: Abhishek Srivastava, MD, Society of Urologic Oncology Fellow, Fox Chase Cancer Center, Fox Chase Cancer Center, Philadelphia, PA Twitter: @shekabhishek at the American Urological Association's 2019 Annual Meeting (AUA 2019), May 3 – 6, 2019 in Chicago, Illinois


