Anatomically speaking, there have been a few very nice mapping studies that have clearly delineated where the nerves run, in relation to the prostate itself. First, there are no nerves in the prostatic capsule itself. Next, beyond the “veil of Aphrodite”, the bundle of nerves that run lateral to the prostate (originating from near the seminal vesicles and base of prostate and running distally but staying posterior to the prostate/urethra), there is also a proportion of nerves that runs anteriorly. Alsaid et al. demonstrated this nicely, as seen below:

In between active surveillance and definitive therapy, there is a window of opportunity – and focal therapy is starting to fill in that gap. Focal therapy comes in many forms, primarily in the form of energy delivered via transrectal ultrasound probes into the prostate. However, a few groups have now begun to consider surgical focal therapy options – including the recent paper by Villers et. al on the role of partial prostatectomy for anterior tumors.
In an effort to better understand the role of surgical options for partial prostatectomy / focal prostatectomy, Menon’s group completed a thought experiment (an IDEAL phase 0 study). They selected patients who were focal therapy candidates (according to Ahmed et al. Lancet Oncology, 2012) – Gleason score <= 4+3, stage <= T2. They then did a mapping study to determine how much prostate cancer they would miss or treat if they sequentially treated more of the prostate beyond the index lesion. They mapped the prostate of patients with similar inclusion criteria and came up with the following:

In this patient, if they treated the index lesion in the right base with traditional therapies, such as focal hifu or hemiablation, they would still be missing significant amount of cancers, including significant cancers. The rim of yellow is also a rim of tissue that may be missed as they try to spare the nerves. Hence, focal therapy has limitations when done by the transrectal approach.
In contrast, they developed the concept of a Precision Prostatectomy (MPP). Here is what it would look like in this patient:

They would be leaving one of the seminal vesicles with the neurovascular bundle, leave the anterior nerves. They would be missing ~30% of cancers, of which maybe ~10% may be clinically significant. In order to reduce this, they actually do focused pre-operative biopsies and intra-operative biopsies to help ensure that they aren’t. In doing so, they 1-1.5 cc of prostate and prostate capsule are preserved (~5%). This has been confirmed on pre- and post-operative imaging
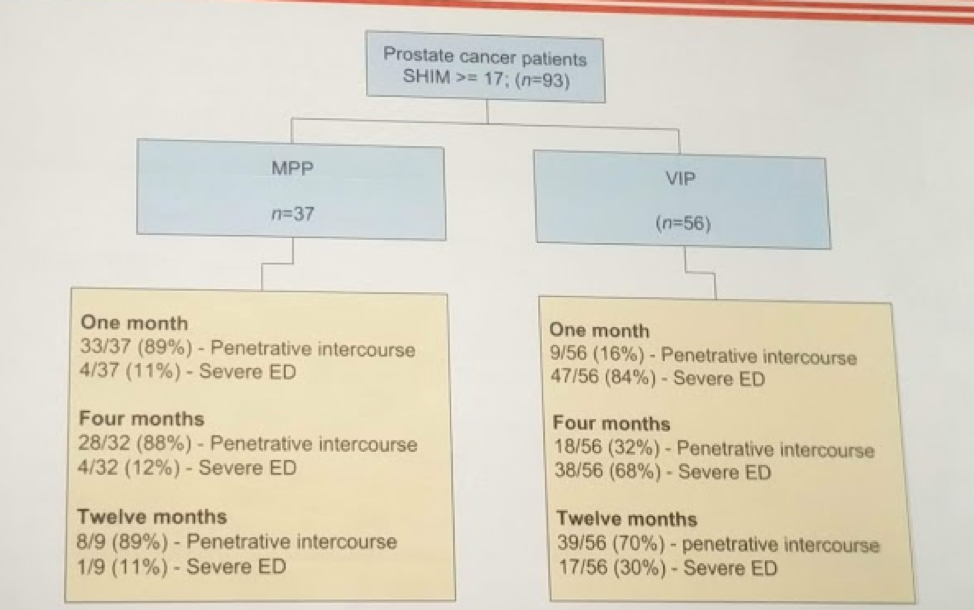
He presented some brief early outcomes from this approach. Unlike radical therapies such as radical prostatectomy and EBRT, there is minimal impact on erectile function or urinary continence, even in the immediate post-operative period.
Below is the results of the erectile function outcomes – of note, the 12-month numbers for radical prostatectomy approach those of MPP. So, given 24 months, would the gap be small enough to still warrant MPP approach?
In terms of PSA outcomes, similar to focal therapy, PSA values drop, but not to undetectable. Mean PSA nadir (usually by 4 months, not by 1 month) is ~0.7. They then manage the patients by Phoenix criteria (BCR is PSA reaches 2 above nadir).
This is definitely innovative. There remain oncologic concerns, but they continue to follow the patients with mapping studies. Further research is required, but Dr. Menon continues to push the boundaries of robotic prostatectomy
Presented by: Mani Menon, MD Henry Ford, Detroit, MI
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, @tchandra_uromd at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA


