Her three main focuses were systemic therapy advances in RCC management, the role of cytoreductive nephrectomy in RCC, and biomarkers in RCC.
Systemic Therapy Advances in RCC
There have been numerous trials reported in the past few years and the playing field for systemic therapy for RCC is full of novel agents. The current dilemma is patient selection and agent selection.
This slide (from Nature Reviews) highlights the rapid growth in this space from the “dark ages” (1990’s-2005) when High-dose IL2 and IFN-alpha were the only main options, to the current “Golden age” (2015-2025), when numerous agents have been approved. The goal moving forward into the “Diamond age” (2025-2035) is new drugs, drug combinations, drug sequencing, vaccinations, and precision therapy.
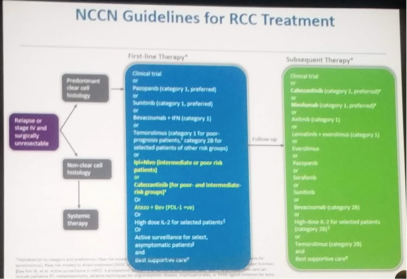
Unfortunately, or fortunately, this is the current NCCN landscape – so many “equivalent” options for first and second-line therapy for mRCC.
I particularly liked this slide highlighting what medical oncologists currently consider when making a decision about drug therapy for these patients.
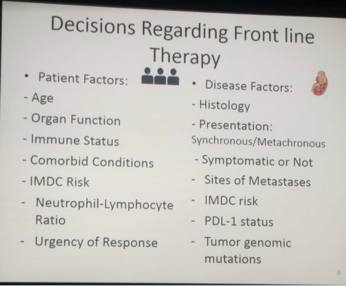
TARGET trial (Eisen JNCI 2008) demonstrated that age was not necessarily an issue for targeted therapy – patients older than 70 appeared to gain the same benefit as patients under 70.
Rini et al. (Lancet Oncology 2017) demonstrated that active surveillance was a mixed bag in this population – safe for some but not others, as the disease kinetics varied from patient to patient and could change within a single patient.
Site of metastatic disease also plays a role in decision making process.
Lung mets: most common site of metastases. Excellent prognosis. Lung-only mets – consider IL-2.
Pancreas: 10% of patients. Good prognosis.
Bone: Consider to have worse prognosis. Cabozantinib seems to have particular efficacy in this setting
Brain and Liver mets: Poorer prognosis, especially brain metastases.
Brain mets from solid malignancies is an area we still treat very poorly and patients deserve better options. Mainstay of therapy is surgery and/or radiotherapy. CXCR4 is a target overexpressed in brain mets and may be worth exploring from a therapeutic standpoint.
Some recent advances in RCC systemic therapy management include:
1. CABOSUN – phase III trial of cabozantinib vs. sunitinib in intermediate/poor risk RCC patients. Cabo had 3.3 month PFS survival benefit and potentially early hint of OS benefit. Bone lesions in particularly responded well to Cabo.
2. CheckMate 214 – phase III trial of Iplimumab/Nivolumab (combined I/O therapy) vs. sunitinib for mRCC. Appeared to have a OS and PFS benefit, particularly in patients who were PD-L1 > 1%. However, based on this, patients with PD-L1 <1% should not be excluded from therapy.
3. InMotion 151 – Bevacizumab/atezolizumab vs. sunitinib – Bev/atezo appeared to provide PFS benefit in the PD-L1+ patients.
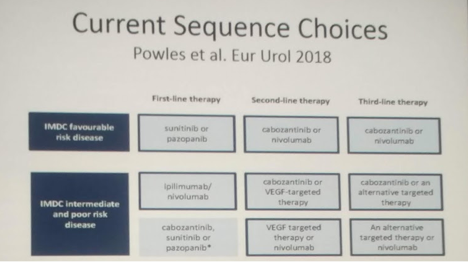
A recent publication by Powles et al (EU 2018) summarizes the current sequencing suggestions. Patients should be treated based on IMDC risk stratification.
Cytoreductive nephrectomy
Next she focused on the role of cytoreductive nephrectomy. This has been a moving target, especially in the targeted therapy era. Originally introduced in the IL-2/IFN-alpha era where it was demonstrated to have overall survival benefit, this is less clear in the current era.
In real-world, population level analyses, cytoreductive nephrectomy is utilized in approximately 36% of patients (Vaishampayan KCA 2017). Hence, clinical trial data which is carried out in patients s/p nephrectomy >90% of the time, does not represent the real world patient.
In retrospective series, CNx demonstrates OS benefit – but is plagued by selection bias. Even these studies, though, note that it often does not have a benefit in patients with IMDC 3+ scores (poor risk).
Clinical trial data is slowly being published.
SURTIME was the first to report. Randomized patients to sunitinib upfront with delayed CNx vs. CNx upfront. Primary outcome OS. Patients with deferred CNx actually did slightly better – and indeed, this was definitely non-inferior.
She highlighted the fact that the other phase III clinical trial in this setting (CARMENA) out of Europe will be reported their results as a late-breaking abstract on Sunday. Full results on Urotoday!
Final considerations:
Both retrospective and prospective series agree that bulky, poor risk patients do not benefit from upfront CNx – systemic therapy needed
No evidence at this point for role of CNx with I/O therapy – indeed, may be beneficial to leave the primary in to prime the system!
Surgical feasibility and bulk of disease outside the kidney should be considered
PROBE trial – trial that she and Hyung Kim are starting. Phase III clinical trial assessing the sequencing of I/O combination therapy pre- and post-cytoreductive nephrectomy in advanced mRCC. May help address this question!
Biomarkers for RCC management
Lastly, she briefly touched on this topic. Many of these topics were reviewed by the other speakers, so I won’t touch on all of them in depth.
1. PBRM1 and BAP1 – mutations that have significant clinical implications. They may be prognostic, predictive or both.
2. VEGF responsiveness and NLR (neutrophil to lymphocyte ratio) – her work in this area notes that patients who had a strong response to VEGF therapy (>6 months) or had high NLR were less like to respond to subsequent I/O therapy
3. IMDC – patient risk stratification tools. This is one amongst many, but one most often used. Dr. Heng will talk more about it.
Unfortunately, there is a paucity of biomarkers. Due to tumor heterogeneity, one biomarker will not be sufficient for RCC. Ultimately, will be a combination of markers.
Presented by: Ulka Vaishampayan, MD
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 2018 ASCO Annual Meeting - June 1-5, 2018 – Chicago, IL USA


