Just last month, a group out of the Netherlands presented the data of the first multi-center prospective trial in this disease space – focusing on the role of XRT (without pelvic node radiation) in patients with large volume metastatic disease. As expected, there was no benefit to primary XRT. However, the study was limited to patients with high volume disease and elevated PSAs. Full coverage of the study can be found at: https://www.urotoday.com/conference-highlights/aua-2018/aua-2018-prostate-cancer/104257-aua-2018-a-prospective-randomized-controlled-trial-evaluating-overall-survival-in-patients-with-primary-bone-metastatic-prostate-cancer-mpca-receiving-either-androgen-deprivation-therapy-adt-or-adt-combined-with-concurrent-radiation-therapy-to-the-prostate-final-data-from-the-horrad-trial.html
In this abstract, the authors from a single institution present their results of primary XRT in patients with de novo metastatic hormone-sensitive prostate cancer. The study population included men referred between 2005 and 2015 and treated initially with androgen deprivation therapy. Patients were eligible for inclusion if they received 1) prostate RT with biologically effective dose at least that of a course of 40 Gy in 15 fractions or 2) no prostate RT. Functionally this served as two arms, but in a retrospective nature. The association between receipt of prostate RT and OS was studied. The primary outcome was overall survival.
The retrospectively identified 304 eligible men. Prostate RT was received in 105 cases, the remaining 199 did not receive RT. Decision management was at the discretion of the treating physician.
Median age at diagnosis was 75 years (IQR, 67-82 years). Median follow-up was 72.2 months.
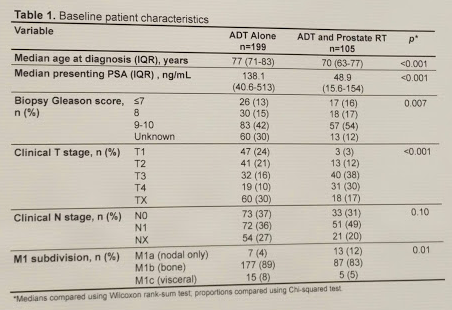
These are clearly not balanced groups – patients who received prostate RT were less likely to have M1b/c disease, less likely to have N1 disease, had much lower median PSA, and were much younger!
On univariate analysis, prostate RT was associated with improved OS (HR 0.62, 95% CI 0.46-0.84, p = 0.002). 2-year and 5-year OS was 74.7% and 41.8% respectively in those receiving prostate RT and 56.9% and 27.6% respectively in those not receiving RT. Median OS in those receiving RT was 48.3 months versus 29.2 months in those not receiving RT.
Importantly, in a multivariate Cox model taking account of age at diagnosis, year of diagnosis, presenting PSA, T stage, N stage, and M1 subdivision, RT remained associated with improved survival (HR 0.64, 95% CI 0.43-0.96, p = 0.033).
One interesting analysis they did was look at patients that lived at least 1-2 years, and even in these subsets, patients who received RT had better OS.
Based on this, consistent with other retrospective series and population-based analyses, local definitive therapy in the setting of de novo metastatic prostate cancer may have some OS benefit. This cohort represents the largest single-center experience of primary tumor-directed RT in mPCa reported to date. The observed 19-month absolute difference in median OS is clinically significant.
They note the major limitations, beyond being a retrospective series (with its inherent limitations and selection bias) - they could not account for performance status, volume of metastatic disease, comorbidities, receipt of systemic therapies, and other potential confounders.
Only large-scale RCTs will be able to definitively assess the value of prostate RT in this setting. These are already underway and will be hopefully reporting soon!
Presented by: Scott Carlyle Morgan, MD
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 2018 ASCO Annual Meeting - June 1-5, 2018 – Chicago, IL USA


