BERKELEY, CA (UroToday.com) - How many of us are distressed by nocturia, the concern of a person, young or old, who must awaken one or more times at night to void;[1] and how do we treat it as medical professionals?
According to an epidemiological survey conducted in Japan, 10 to 30% of men and women under 65 years old and 40 to 80% of those over 65 years old have nocturia,[2] and in these older people, nocturia increases the risk of hip fractures and significantly reduces survival. For these patients, the ultimate goal is to treat the nocturia so that they can get enough high-quality sleep and have fewer voids, day or night; thus, improving their quality of life (QOL).
However, before we can improve the QOL of the patient, we must find the cause of the nocturia. Patients with nocturia may have one or more medical conditions: polyuria, bladder storage disorder or a sleep disorder, which are dependent. When patients with nocturia present with lower urinary tract symptoms and urgency, OAB is the diagnosis, and an antimuscarinic drug is the first choice for treating OAB.
Our subgroup analysis was the first of its kind to study the effect of solifenacin on nocturia and sleep by using bladder diary results for 3 consecutive days.[3] Even though diary entries were sometimes incomplete, because of the troubling nature of the collected data, the information proved extremely valuable. From the diaries, we could obtain frequency of waking to void, volume of each nighttime void and the first morning void, hours of undisturbed sleep (HUS) before the first nighttime void. The subgroup analysis is the first report of the impact on sleep evaluated by bladder diary.
Over 12 weeks, 962 patients taking solifenacin 10 mg had 0.46 fewer episodes of nocturia. The mean change of nighttime volume voided per micturition was 41 mL, which was significantly greater than the 13 mL for placebo. In addition, solifenacin 5 mg had 0.42 less episodes of nocturia with a nighttime volume voided per micturition of 30 ml. Both 5 and 10 mg doses prolonged HUS by 59 and 60 minutes, while for placebo it was only 33 minutes (see Figure 1).
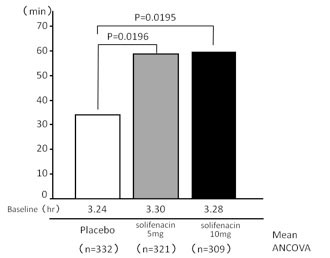
Figure 1. Mean change in hours of undisturbed sleep (HUS)
of solifenacin treatment versus placebo.
In the human sleep cycle of healthy adults, deep sleep (slow wave sleep) occurs about 2 to 3 times per night, usually earlier in the cycle. Allowing uninterrupted sleep at the beginning of the cycle seems to correlate with quality of sleep. If treatment prolongs HUS, then we have a better chance at helping patients improve their quality of sleep.
We should ask why solifenacin improves nocturia. We do know that desmopressin does improve symptoms of nocturnal polyuria, measured by the reduction in the nocturnal polyuria index (NPi). Desmopressin inhibits the production of urine, so with less urine in the bladder, the person does not wake to void. Solifenacin, on the other hand, increases the functional bladder capacity, and in the subgroup analysis, it significantly increased nighttime voided volume per micturition after 12 weeks, compared to placebo. With an increased bladder capacity, the patient may not sense the need to empty the bladder early in the night and can sleep longer. Thus, the mechanism of solifenacin in reducing voiding frequency is entirely different from that of desmopressin.
Reducing nighttime urinary frequency, by treating OAB with solifenacin, and in turn improving the quality of sleep by prolonging HUS were our goals. We hope that, with greater interest and cooperation from patients to collect data for a trial, we will be able to provide, without a doubt, the value of solifenacin in improving the quality of sleep and quality of life of patients with nocturia.
References
- Abrams P, Cardozo L, Fall M et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Subcommittee of the International Continence Society. Neurourol Urodyn 20021 21: 167.
- Homma Y, Yamaguchi O, and Hayashi K: Epidemiologic survey of lower urinary tract symptoms in Japan. Neurogenic Bladder Society Committee. Urology 20061 68: 560.
- van Kerrebroeck P, Abrams P, Chaikin D et al. The standardisation of terminology in nocturia: report from the Standardisation Subcommittee of the International Continence Society. Standardisation Subcommittee of the International Continence Society. Neurourol Urodyn 20021 21: 179.
Written by:
Osamu Yokoyama, MD, PhD as part of Beyond the Abstract on UroToday.com. This initiative offers a method of publishing for the professional urology community. Authors are given an opportunity to expand on the circumstances, limitations etc... of their research by referencing the published abstract.

UroToday.com Overactive Bladder (OAB) Section


