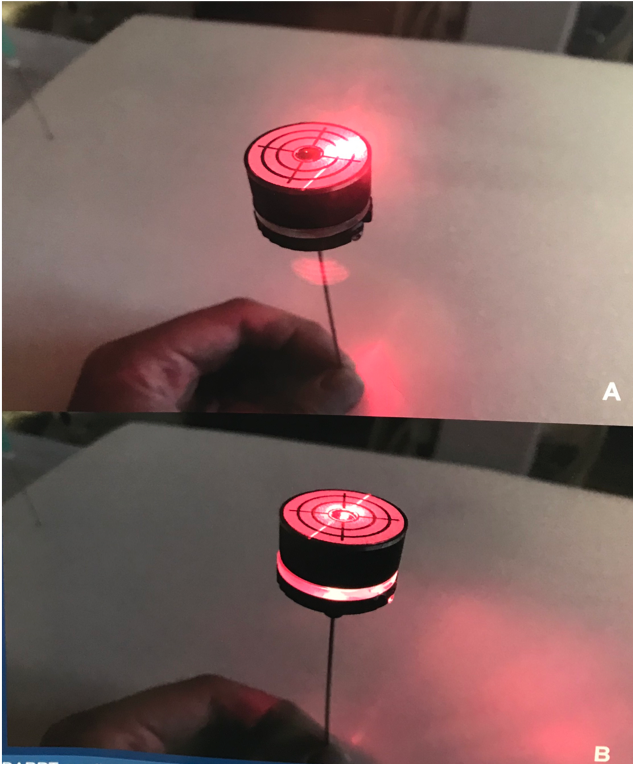
Figure 1: The laser direct alignment radiation reduction technique (DARRT) technique. A, The DARRT needle prior to alignment. B, The DARRT needle after proper alignment of the C-arm laser.
In order to test the efficacy of the DARRT and LRT techniques, six attending surgeons, six residents, and ten medical students were asked to gain access to the upper, middle, and lower poles of a phantom renal model with each of the three previously described techniques. The primary data endpoints from the experiment included total fluoroscopy time, total needle insertion time, number of punctures, and number of course corrections.
Following the completion of this in vitro trial, there was a significant reduction of fluoroscopy times in both the DARRT and LRT access techniques compared with the conventional access technique (Figure 2). The DARRT technique led to an average of 89.8% decrease of fluoroscopy time while the LRT led to an average reduction of 81.8% when compared to the conventional technique. Interestingly, Dr. Hajha noted that there was minimal differentiation in the fluoroscopy times between all three skill level groups using the LRT and DARRT techniques, insinuating that the technology has a relatively low learning curve and can be used effectively by surgeons of any experience level. However, there was a significant increase in time for the DARRT and LRT techniques (36.83 and 33.17 seconds, respectively) as compared to the conventional access technique (25.67 seconds). There was no significant differences between any of the techniques in regard to number of course corrections or number of necessary punctures to reach the desired calyx.
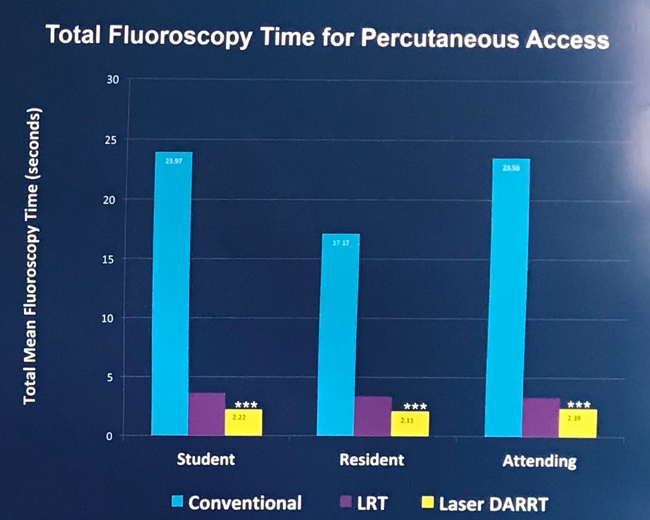
Figure 2: Fluoroscopy times for all three access techniques, separated by surgeon skill level. Of note, the DARRT and LRT techniques showed significantly fewer fluoroscopy times than conventional access for all three skill levels.
Dr. Hajha concluded his presentation by reiterating the necessity for rethinking the way percutaneous access tracts are created due to the great risk that comes with excess fluoroscopy. He admitted the sole drawback of the new techniques was the increase of access times, however, he stated that the low-radiation aspects of these novel techniques outweigh the small additional time necessary to gain access. As such, he additionally restated that this new technology can reduce fluoroscopy exposure for the patient as well as the staff without the need for repeat procedures.
Presented by: Dr. Mohammad Hajha
Authors: Mohammad Hajha, Michael Wilkinson, Jonathan Ewald, Shawn Engelhart, Hillary Wagner, Julie W. Cheng, D. Duane Baldwin
Affiliation: Loma Linda University Health, Department of Urology, Loma Linda, CA
Written by: Zachary Valley, Twitter: @ZacharyAValley, Department of Urology, University of California-Irvine, medical writer for UroToday.com at the 36th World Congress of Endourology (WCE) and SWL - September 20-23, 2018 Paris, France


