(UroToday.com) In a plenary session at the Society of Urologic Oncology Annual Meeting focused on early prostate cancer diagnosis and treatment, Dr. Caroline Moore and Dr. Daniel Spratt provided a point/counterpoint debate on the role of focal therapy for localized prostate cancer. Beginning first, Dr. Moore argued that focal therapy should be considered.
Dr. Moore began by discussing traditional, whole gland approaches to prostate cancer treatment which include active surveillance, surgery, and radiotherapy. Notably, active treatment with either surgery or radiotherapy is associated with meaningful rates of complications: one in 10 men treated surgically will experience a severe genitourinary complication and a comparable number treated with radiotherapy will have a severe gastrointestinal complication in the two years following treatment. Additionally, both treatment approaches adversely affect sexual, urinary, and bowel function. Further, highlighting data from MSKCC, she emphasized that erectile function following radical prostatectomy has not improved over the last decade up to 2015 at centers of excellence.
She emphasized that, over the past 5 to 10 years, there have been dramatic changes in the diagnostic paradigm for prostate cancer with increasing utilization of multiparametric magnetic resonance imaging (mpMRI). This approach allows for anatomically selective detection and diagnosis of prostate cancer, with preferential identification of clinically significant disease.
She emphasized that we all make choices, based on prior experience, knowledge of what outcomes might be, and personal preference. In the context of prostate cancer treatment, Dr. Moore emphasized that both the patient to be treated and the physician offering treatment influence this process, with consideration of tumor characteristics, patient characteristics (comorbidity, baseline function, and preferences regarding treatment duration and follow-up), along with the availability of treatment options. In terms of tumor characteristics, she emphasized the importance of location, grade, and visibility on mpMRI.
Considering functional outcomes, Dr. Moore emphasized data from the UCL Focal HIFU trials. In two publications, they have shown that continence is exceptionally well preserved with 1 in 100 men requiring pads for leakage. Further, erectile function is relatively well preserved with 2 of 3 men with natural erections prior to therapy maintaining this at 12 months and the remainder requiring medical therapy.
In terms of oncologic outcomes, among more than 1000 men treated with focal or Hemi-ablation using HIFU, only 3.8% of patients (39 of 1032) underwent radical therapy during follow-up, despite 80% of the cohort comprising patients with Gleason 3+4 (grade group 2) disease. This, in fact, mirrors their overall treatment cohort in which the majority of patients receiving focal HIFU have Gleason 3+4 disease with a relatively small cohort of patients with Gleason 6 or Gleason 4+3 disease. Over time, the proportion of patients being treated who have Gleason 6 disease has been decreasing.
While less than 4% of men underwent radical therapy during follow-up, 20% required a second focal treatment including focal HIFU, whole gland HIFU, or focal cryotherapy. Further, another 2% of men underwent other therapies including androgen deprivation monotherapy.
She did, however, emphasize that Gleason grade is prognostic of outcome: patients with Gleason 4+3 disease have a higher likelihood of retreatment or radical therapy. Thus, this is used more sparingly and among patients who are older or with more comorbidity.
Additionally, she emphasized that there is a learning curve and, over time, retreatment rates have been decreasing. This likely reflects optimization of patient selection as well as increased operator experience.
She further highlighted data using a propensity score-matched approach of observation data to compare radical prostatectomy and focal therapy (using HIFU or cryotherapy) on the basis of tumor volume and Gleason grade. Considering 3-, 5-, or 8-year failure-free survival, Dr. Moore emphasized that there is little difference between these two treatment approaches, among appropriately selected men.
Dr. Moore highlighted that, in the course of going through the preference-sensitive decision-making process for patients with localized prostate cancer, that we should weigh both the outcomes and processes involved.
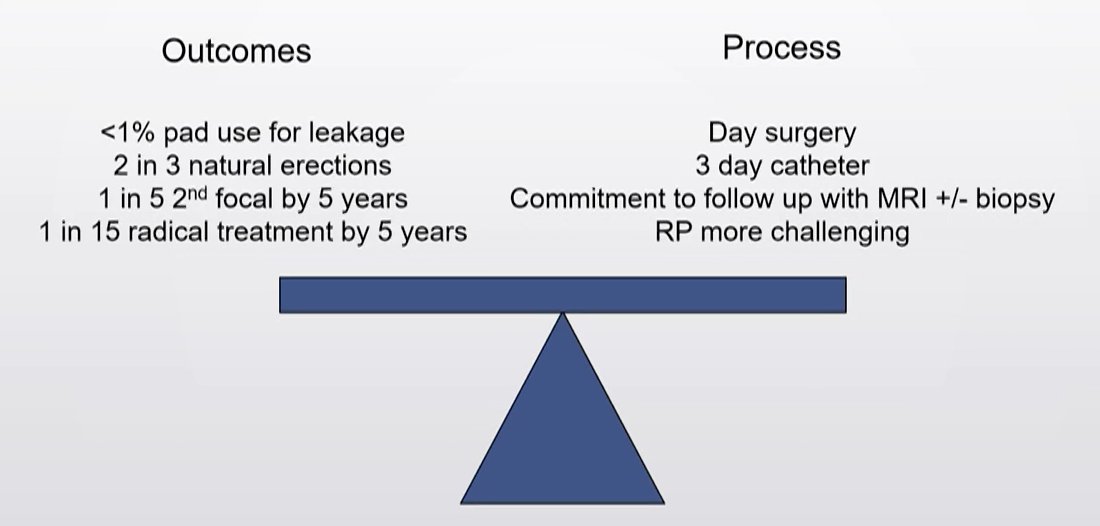
In that context, she posited that focal therapy offers advantages in functional outcomes, similar salvage treatment rates, and the opportunity to offer smaller treatments for smaller tumors.
Presented by: Caroline Moore, MBBS, MD, FRCS, Division of Surgery and Interventional Medicine, University College London