(UroToday.com) In a plenary session of the Society of Urologic Oncology Annual Meeting focused on transperineal prostate biopsy, Dr. Jonathan Shoag discussed whether a transperineal biopsy should become the standard of care for patients undergoing prostate biopsy.
Following Dr. Kaye’s presentation in support of transrectal ultrasound biopsy (TRUS) as the standard of care, Dr. Shoag argued that transperineal biopsy should be considered the standard of care.
Dr. Shoag began by arguing that this argument parallels the work by Lister and colleagues distinguishing between antisepsis which seeks to destroy germs by washes and sprays from asepsis in which a sterile environment, free of germs, is created.
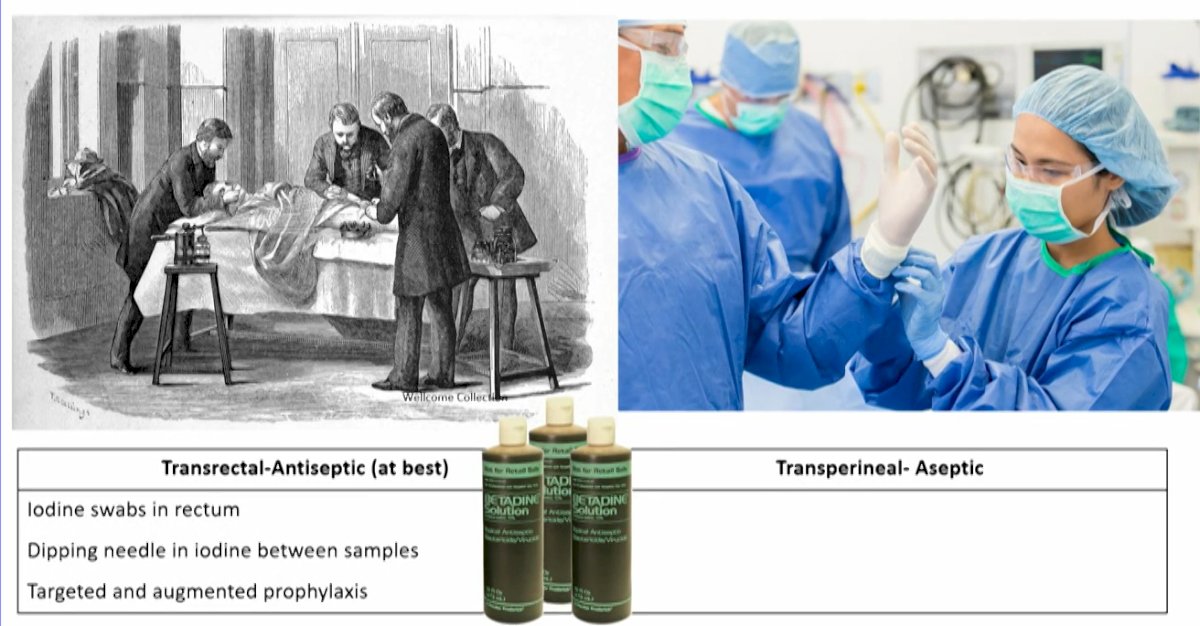
To this end, Dr. Shoag argued that, when we can use an aseptic procedure, we should. Further, this is especially true for common procedures with relatively high infection rates. Additionally, he suggested that we may potentially improve prostate cancer screening and early diagnosis with the use of a transperineal approach.
Citing the National Cancer Institute, Dr. Shoag defined standard of care as “treatment that is accepted by medical experts as a proper treatment for a certain type of disease and that is widely used by health care professionals. Also called best practice, standard medical care, and standard therapy.” To this end, he emphasized that level 1 evidence from phase III trials is not required to meet this bar.
Summarizing the existing data, Dr. Shoag argued that transperineal biopsy has a much lower infection rate, equivalent cancer detection rate, comparable pain when performed in office, and a higher urinary retention rate that may be mitigated by the use of the freehand technique.
In terms of arguments for transrectal biopsy, Dr. Shoag argued that “workflow” advantages really mean reimbursement considerations and that the learning curve necessary for transperineal biopsy translates simply to a time investment for physicians. Additionally, the additional equipment needed means that our institutions need a resource investment to move from transrectal to transperineal approaches. He, therefore, argued that none of these rationales benefit an individual patient.
He further argued that currently, existing challenges with transperineal biopsy do not necessarily support the transrectal approach as the standard of care. To this end, the EAU guidelines suggest transperineal biopsy may be considered first choice, despite considerable limitations to the data. Further, issues such as obtaining equipment, competing techniques, reimbursement, and time considerations similarly affected the uptake of MRI-targeted biopsy adoption, though this has now become widely utilized.
Dr. Shoag further emphasized that transperineal biopsy is “straightforward” to learn. He highlighted that this approach should be the standard of care, and is in some jurisdictions. While many of the reasons supporting transrectal biopsy are pragmatic, he suggested that transperineal biopsy is an easy way to increase the benefit/harm ratio of early prostate cancer detection. He closed by quoting Dr. Johann Mikulicz-Radecki who said “it can be demanded of us that we improve as much as possible the arrangements for the safety of the people who are entrusted to us.”