(UroToday.com) The Society of Urologic Oncology (SUO) 2021 annual meeting in Orlando, FL hosted a debate regarding the role of pelvic lymph node dissection (PLND) in prostate cancer presented by Dr. Karim A. Touijer, MD, MPH who had the unenviable task of advocating both for and against this procedure.
Dr. Touijer began his talk by presenting his team’s own published work regarding practice patterns of uro-oncologists in North America. The majority of physicians performing radical prostatectomies [RP] in North America were performing 50-200 per year. Sixty-two percent of the uro-oncologists reported that they were performing PLNDs when indicated, with half of these physicians performing an extensive PLND involving the obturator fossa, external iliac, and hypogastric regions.1 Dr. Touijer went on to present data regarding the evolution of the lethal prostate cancer cell clone that arises from a small, relatively low-grade cancer focus in the primary tumor, and not from the bulk, higher-grade primary cancer or from a lymph node (LN) metastasis resected at prostatectomy.2 This data would dissuade one from performing a PLND at time of RP.2 Furthermore, Dr. Touijer presented data from Memorial Sloan Kettering that evaluated the long-term outcomes of patients with LN disease at time of RP who did not receive adjuvant androgen deprivation therapy with a 10-year probability of freedom from distant metastasis of 65% and freedom from biochemical recurrence of 28%. As more LNs are harvested at time of PLND, the probability of finding a positive LN linearly increases.
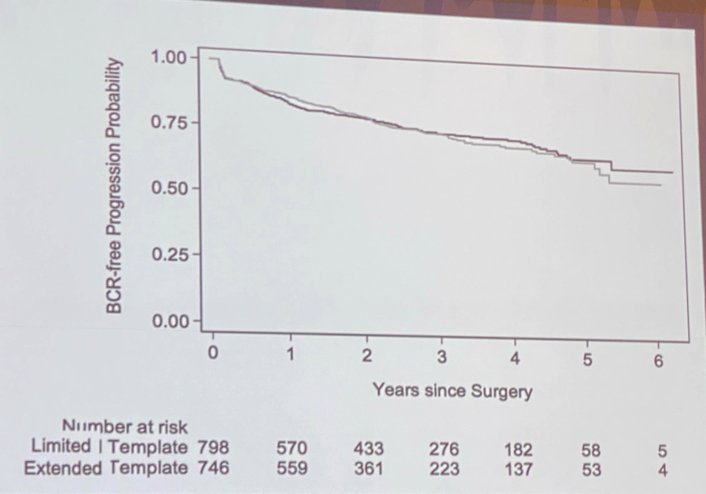
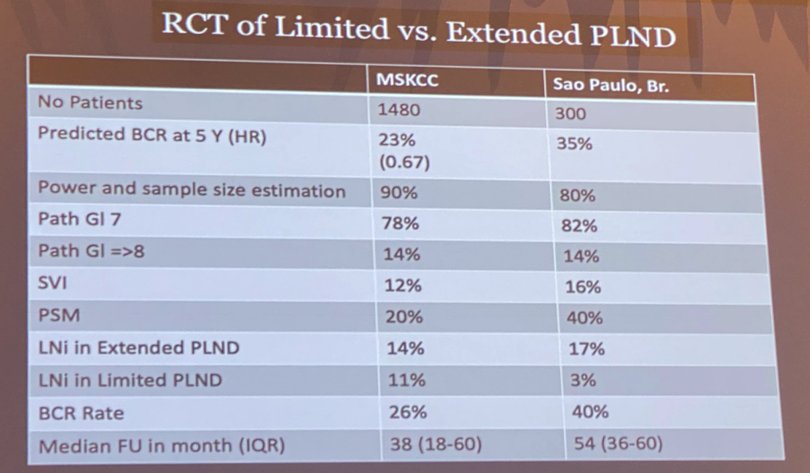
Dr. Touijer went on to present his recently published randomized controlled trial of limited versus extended PLND. The target accrual was 1,400 patients over five years, with a one-year follow-up after the final accrual. The expected recurrence rate at five years was 23%.
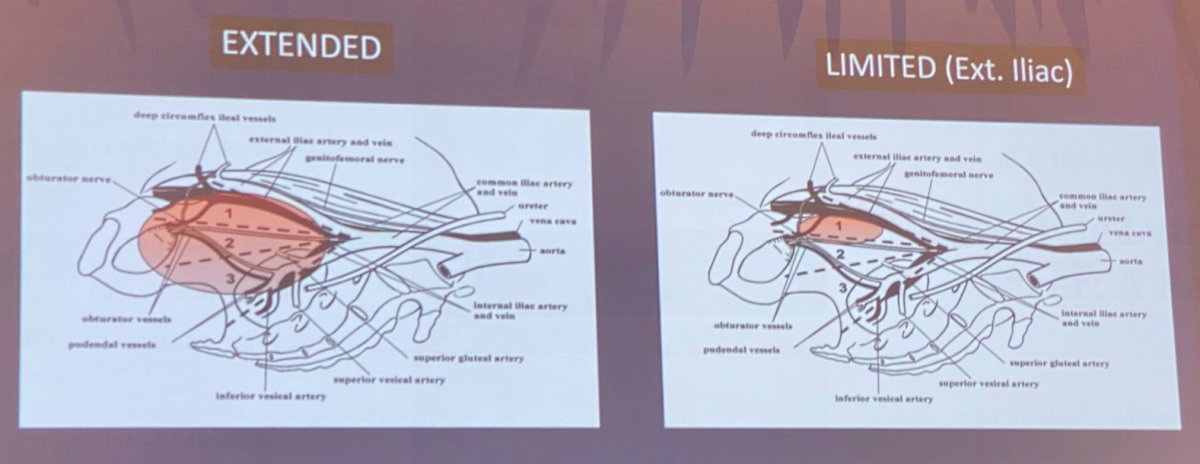
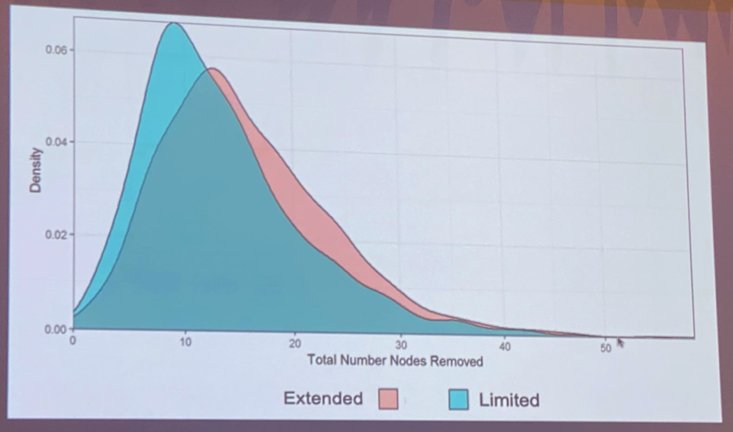
Ultimately, 1,480 patients were accrued (757 in the extended PLND arm and 723 in the limited PLND arm). The primary endpoint was time to biochemical recurrence (BCR). Pathologic nodal disease was present in 103 (14%) extended PLND patients and 81 (11%) limited PLND patients. This was a negative trial with no significant difference in time to biochemical recurrence between the two arms. Subgroup analyses failed to identify a subcohort that would benefit from this procedure.3
Dr. Touijer went on to present data from a Brazilian study that evaluated this same question in 300 patients (150 in each arm). As opposed to the Memorial study that compared extended PLND to limited PLND, this trial compared superextended PLND to limited PLND.
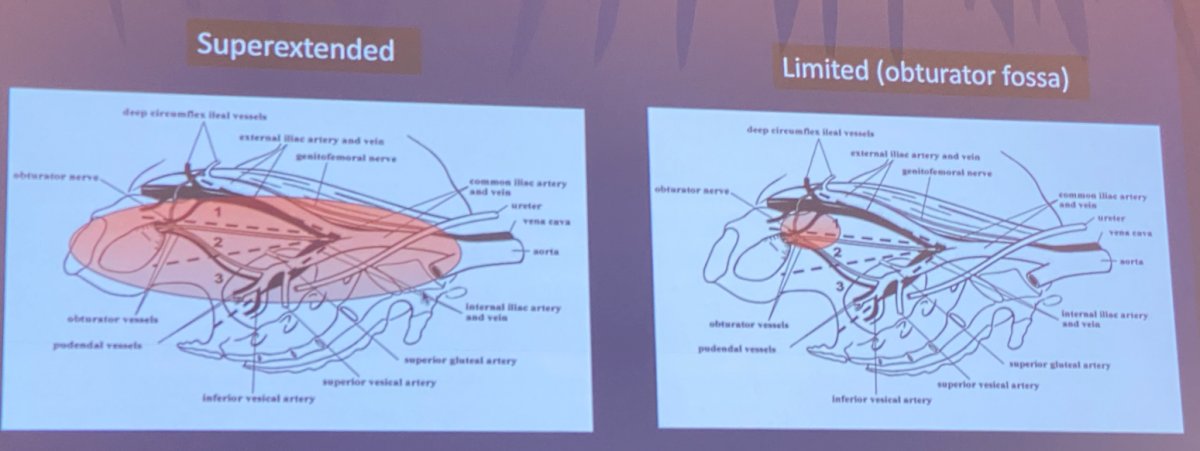
Whereas the positive LN yield was 14% versus 11% in the Memorial cohort, the corresponding rates in the Brazilian trial were 17% and 3.4%, respectively, with the median LN yield 17 in the superextended arm and 3 in the limited PLND arm. Despite this difference, this trial was a negative trial with no significant differences in biochemical recurrence-free rates.4
Dr. Touijer went on to compare this paradigm to that in gastric cancer where a LN dissection has similarly not proven to impact cancer-specific or overall survival despite multiple studies.
The challenges of surgical trials for lymphadenectomies remain:
- Low study power
- Lack of blinding
- Surgical imprecision
Another unique challenge is that 35% of LN metastases fall outside the standard PLND template. He believes that with the advent of PSMA imaging, this false-negative rate is likely to decrease with the improved sensitivity of this imaging tool. However, the sensitivity of PSMA imaging in this cohort remains low with patients having LN diameter less than 2 mm not being detected on PSMA imaging. This sensitivity improves in those with a LN diameter of 2-4.9 mm (60%) and in those with LN diameters of 5mm or larger (86%).
In conclusion, Dr. Touijer believes that:
- PSMA imaging will improve the staging capacity of PLND
- PSMA may not replace PLND
- PLND versus no PLND is a superior trial design to limited versus extended PLND
There are two ongoing trials of PLND versus no PLND in prostate cancer:
- NCT01407263: Memorial Sloan Kettering Cancer Center
- NCT04269512: Hamburg (PREDICT Trial)
Presented by: Karim A. Touijer, MD, MPH, Associate Attending Surgeon, Memorial Sloan Kettering Cancer Center, Professor of Urology at The Weill Medical College of Cornell, New York, NY
Written by: Rashid Sayyid, MD, MSc – Urology Chief Resident, Augusta University/Medical College of Georgia, @rksayyid on Twitter during the 2021 Society of Urologic Oncology (SUO) Winter Annual Meeting, Orlando, FL, Wed, Dec 1 – Fri, Dec 3, 2021.
References:
- Touijer KA, Ahallal Y, Guillonneau BD. Indications for and anatomical extent of pelvic lymph node dissection for prostate cancer: practice patterns of uro-oncologists in North America. Eur Urol Oncol. 2013 Nov;31(8):1517-21.
- Haffner C, Mosbruger T, Esopi D. Tracking the clonal origin of lethal prostate cancer. J Clin Invest. 2013 Nov;123(11):4918-22.
- Touijer KA, Sjoberg DD, Benfante N, et al. Limited versus Extended Pelvic Lymph Node Dissection for Prostate Cancer: A Randomized Clinical Trial. Eur Urol Oncol. 2021 Aug;4(4):532-539.
- Lestingi JFP, Guglielmetti GB, Trinh Q, et al. Extended Versus Limited Pelvic Lymph Node Dissection During Radical Prostatectomy for Intermediate- and High-risk Prostate Cancer: Early Oncological Outcomes from a Randomized Phase 3 Trial. Eur Urol. 2021 May;79(5):595-604.