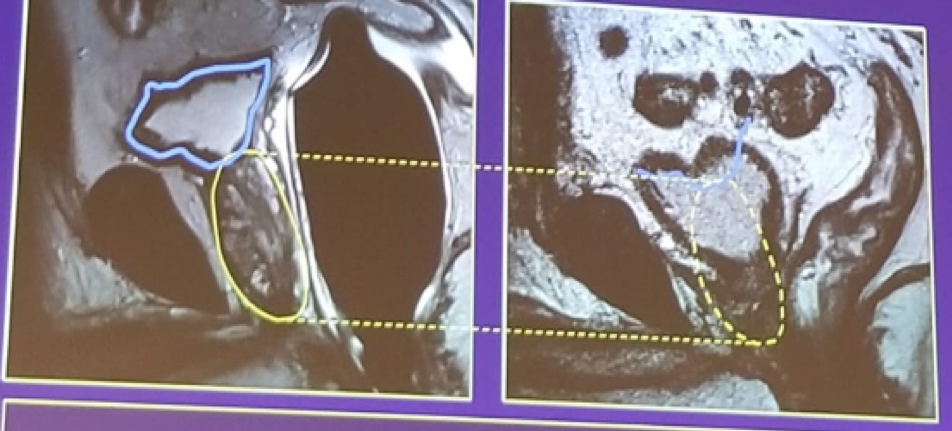
Figure 1 - Bladder descent post-prostatectomy:
Post-prostatectomy recurrence is defined as two consecutive PSA rises above 0.2 ng/ml. The recurrence can either be local or distant. In local recurrence, there are usually low PSA values and long PSA doubling time. The local recurrence predominantly occurs in the perianastomotic (52%) and retro-vesical area (20%), followed by the bladder neck area (16%), and circumferential areas (12%). 2The overall rate of MRI-detectable lesion in men referred for salvage radiotherapy is 24%. 3 When stratifying the MRI detection rate by PSA values, a clear trend is evident with higher PSA values correlating to a higher rate of MRI-detection (PSA <0.2 ng/ml – 8% detection rate, 0.2-0.3 ng/ml – 18% detection rate, 0.31-0.72 ng/ml – 35% detection rate, and >0.72 ng/ml – 38% detection rate).When assessing the performance of the specific MRI phases for this state of postsurgical recurrence, T2 imaging has a sensitivity of 48-61%, and a specificity of 52-82%. 4 The diffusion-weighted imaging (DWI) has a sensitivity of 94-98% and specificity of 92-96% and is correlated with the aggressiveness of the recurrence.5 The dynamic contrast enhancement (DCE) demonstrates an earlier and faster enhancement than fibrosis, with a sensitivity of 88% and a specificity of 87%.6. Therefore, according to the speakers, the recommendation is to perform T2+DWI+DCE MRI when there is suspicion of a local recurrence postoperatively, and when PSA is between 0.2-1 ng/ml (increasing accuracy with increasing PSA).
Next, the changes occurring in the prostate after radiotherapy were discussed. Following either external beam radiotherapy or brachytherapy, one could expect to find inflammation, glandular atrophy, fibrosis, and prostate shrinkage. The MRI demonstrates diffusely decreased signal intensity and loss of zonal anatomy, as can be seen in figure 2. In this state of diagnosing postradiotherapy recurrence, T2 weighted MRI has a sensitivity of 26-44% and a specificity of 63%-86%.7 Due to this poor performance, other MRI phases are required. The DWI demonstrated a lower ADC than surrounding irradiated tissue, with a sensitivity of 49-97% and a specificity of 91-93%.8 The DCE demonstrates early enhancing areas, with a sensitivity of 70%-97%, and specificity of 73%-85%9 Similarly to postprostatectomy, the recommendation is to perform T2 + DWI +DCE when there is suspicion of recurrence in a postradiotherapy patient.
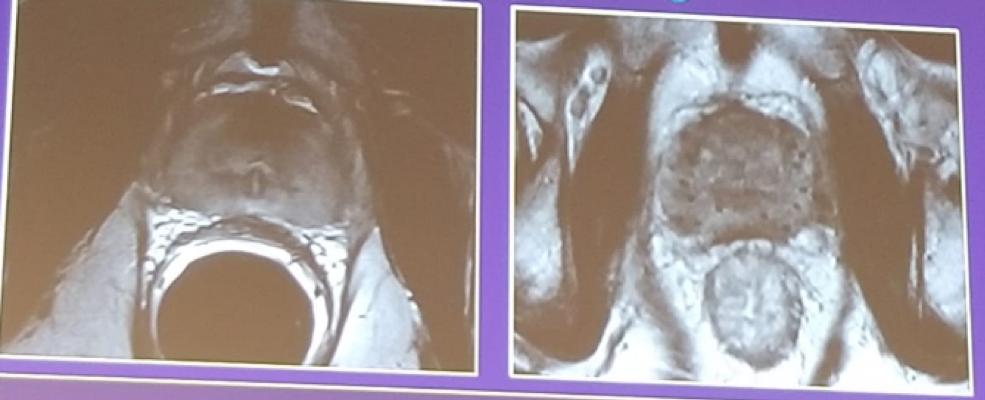
Figure 2 – Postradiotherapy MRI demonstrating diffusely decreased signal intensity and loss of zonal anatomy:
The speakers concluded their talk mentioning the role of the positron emission tomography (PET)-based imaging. In recent years, PET/CT imaging has been used more prevalently in prostate cancer and could offer a promising alternative to conventional imaging for characterizing the true extent of the recurrent prostate cancer. In a recently published meta-analysis including over 3200 patients who underwent PET imaging using the radiolabeled tracers: 11-choline, 18F-FACBC, or 68Ga-PSMA, the reported results were quite promising.10 The sensitivities of these tracers were 80.9%, 79.7%, and 76.4%, for 11-choline, 18F-FACBC, or 68Ga-PSMA, respectively. The respective specificities were 84.1%, 61.9%, and 99.8%. Importantly, the recurrence detection rates ranged between 58%-82%. These results are quite encouraging, but further prospective trials are needed to validate them.
Presented by: Wim Oyen, London, Great Britain and Geert Villeirs, Ghent, Belgium
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the 2nd EAU Update on Prostate Cancer (PCa18)– September 14-15, 2018 – Milan, Italy
References:
1. Sella et al. Am J Roentgenol 2006; 186:539
2. Martino, et al. World J Urol 2011; 29:595
3. Liauw et al. IJROBP, 2013; 85:378
4. Casciani et al. AJR 2008; 190:1187-1192
5. Panebianco et al. Eur Radiol 2012; 23: 1745
6. Yu et al. Cell Biochem Biophys 2015; 72:687
7. Rouviere, et al. Urology 2004; 63: 922-927
8. Kim et al. JMRI 2009; 29:391-397
9. Haider et al. Int J Radiat Oncol Biol Phys 2008; 70: 425-430
10. Sathianathen NJ, et al. World J Urol. 2018