Dr. Roobol notes that patients with low-risk disease are highly unlikely to die of cancer and treatment is focused on avoiding harm. Contrarily, patients with M+ disease are likely to die of cancer and the focus is on prolonging survival. Most importantly, these treatment discussions are all in the balance maintaining the patient’s wishes and quality of remaining life. Treatment choices become more crucial in those cases where the tumor characteristics can be considered as intermediate and life expectancy is approximately more than 10 years.
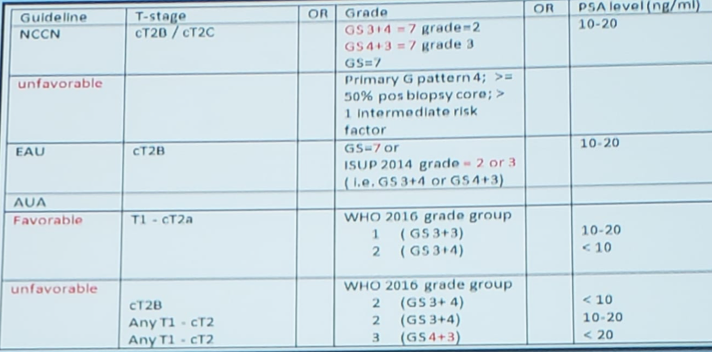
There are several different definitions of intermediate disease, which Dr. Roobol highlights in the following table:
To assess long-term outcomes among men with prostate cancer incorporating information on clinical risk category, Rider et al.1 assessed 15-year mortality for men with prostate cancer treated with noncurative intent among 76,437 cases in the National Prostate Cancer Register (NPCR) of Sweden diagnosed from 1991 through 2009. Patients with a CCI of 0 with low risk (T1-T2 tumor, PSA level <10 ng/ml, and Gleason score ≤6) and intermediate risk (T1-T2 tumor and PSA level 10-<20 ng/ml or Gleason Score 7) prostate cancer had no differences found in observed versus expected all-cause mortality in the low-risk group. Importantly, the observed mortality was only slightly greater in the intermediate-risk group. As has been the dogma among a subset of urologists, and highlighted by Dr. Roobol “the majority of men with low- or intermediate-risk prostate cancer will not die from their disease, even when curative interventions are withheld.”
Importantly, it is crucial to have absolute accuracy regarding prostate biopsy pathology. Looking at the details of the PIVOT trial2, among patients with intermediate-risk prostate cancer, the absolute risk difference in prostate cancer mortality of 4.6% in favor of radical prostatectomy on the basis of local histologic findings changed to 1.3% in favor of observation on the basis of central histologic findings. As Dr. Roobol highlights, not all Gleason 4 is the same. Gleason 4 may include: (i) fused pattern, (ii) ill-formed pattern, (iii) glomeruloid pattern, and (iv) cribriform pattern.
In work from Dr. Roobol’s group, being absolutely sure patients do not have the cribriform or intraductal disease is critical. Among 1,031 patients from the first screening round of the European Randomized Study of Screening for Prostate Cancer (1993-2000), patients who either had invasive cribriform growth pattern or intraductal carcinoma Gleason score 3+4=7 had worse DSS compared to Gleason score 6, whereas those with Gleason score 3+4=7 without cribriform or intraductal components did not (p=0.30)3. Dr. Roobol and her colleagues concluded that men with biopsy negative cribriform/intraductal Gleason score 3+4=7 prostate cancer could be candidates for AS, as these patients have similar survival probabilities to those with Gleason score 6. As a potential caveat, small studies have suggested that cribriform growth patterns are not well visualized on mpMRI, albeit this hypothesis requires further validation.
Dr. Roobol concluded her advocacy for considering AS for men with Gleason 3+4 disease with several take-home messages:
- Based on the current knowledge we can identify patients with Gleason score 3+4 prostate cancer that has a low risk of experiencing progression when not actively treated
- This is not a negligible percentage of all Gleason 3+4 patients
- Gleason 3+4 does not equal immediate active treatment
- At the end of the day, whether to treat or to monitor remains the patient’s choice after a thorough discussion and a shared decision-making process between doctor and patient
Presented by: Monique J. Roobol, Ph.D., MSc, Erasmus University Medical Center, Department of Urology, Rotterdam, The Netherlands
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md, at the 16th Meeting of the European Section of Oncological Urology, #ESOU19, January 18-20, 2019, Prague, Czech Republic
References:
- Rider JR, Sandin F, Andren O, et al. Long-term outcomes among noncuratively treated men according to prostate cancer risk category in a nationwide, population-based study. Eur Urol 2013 Jan;63(1):88-96.
- Wilt TJ, Brawer MK, Jones KM, et al. Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med2012;367:203-213.
- Kweldam CF, Kummerlin IP, Nieboer D, et al. Disease-specific survival of patients with invasive cribriform and intraductal prostate cancer at diagnostic biopsy. Mod Pathol 2016 Jun;29(6):630-636.
Treatment of Gleason 3+4 in a Multidisciplinary Scenario: Focal Therapy
Treatment of Gleason 3+4 in a Multidisciplinary Scenario: Hypofractionation Radiation Therapy
Treatment of Gleason 3+4 in a Multidisciplinary Scenario: Surgery