(UroToday.com) The 2022 ESMO annual meeting included a session focusing on PSMA biology, diagnostics and treatment and a presentation by Dr. Shahneen Sandhu discussing 177-Lutetium (Lu)-PSMA for prostate cancer treatment. Dr. Sandhu noes that the definition of PSMA theranostics is “targeted therapeutic and diagnostic companion,” specifically a 68Ga-PSMA-11 PET/CT + Lu-PSMA therapy. The first major trial utilizing Lu-PSMA in prostate cancer was the TheraP trial.1 This open label, phase II trial evaluated Lu-PSMA vs cabazitaxel for men with mCRPC after docetaxel. To screen into the study, all men had both 68Ga-PSMA-11 and 18F-FDG PET/CT and were required to have high PSMA-expression (at least one site with SUVmax ≥ 20) and no sites of FDG-positive/PSMA-negative disease. All patients had progressive disease with rising PSA ≥20 ng/mL after docetaxel and 91% had received prior enzalutamide or abiraterone. Overall, 200 patients were randomized 1:1 to Lu-PSMA 6-8 GBq every 6 weeks for up to 6 cycles of therapy or cabazitaxel 20 mg/m2 every 3 weeks for up to 10 cycles. Patients were stratified based on disease burden and prior anti-androgen therapy:

Of note, about 1/3 of patients who had registered for the study (91/291) were ineligible prior to randomization, either because of low PSMA expression or FDG discordant disease. The primary endpoint of this study was a PSA decline of 50% (PSA50) and secondary endpoints included PSA-PFS and OS. Baseline characteristics for TheraP were as follows:

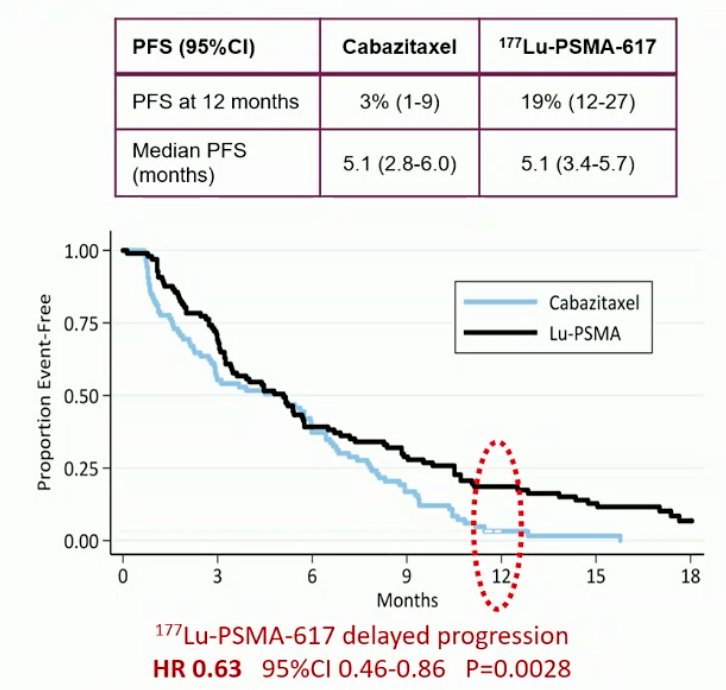
After a median follow up of 13 months, Lu-PSMA significantly improved PSA-PFS compared with cabazitaxel (HR 0.63, 95% CI 0.46 to 0.86):
Additionally, patients treated with Lu-PSMA vs cabazitaxel had a much higher PSA50 rate (66% vs 37%):

Updated analysis of TheraP was presented at ASCO 2022 after a median follow-up of 36 months and PFS continued to favor the Lu-PSMA arm (HR 0.62, 95% CI 0.45 to 0.85). There were no significant differences in restricted mean survival time OS between the two arms (19.1 months in Lu-PSMA arm versus 19.6 months in cabazitaxel arm, 95% CI for difference: -3.7 - +2.7):

Notably, OS was significantly worse in the 61/90 excluded patients with evaluable data, with restricted mean survival time OS of 11.0 months in these patients despite 48% and 5% eventually receiving cabazitaxel and Lu-PSMA, respectively. In terms of the adverse events/safety profile, Grade 3/4 toxicity was seen in 54% of men on cabazitaxel compared to 35% of patients who received Lu-PSMA. Generally, patient reported outcomes from the TheraP trial favored Lu-PSMA over cabazitaxel, specifically for diarrhea, fatigue, and social functioning:

Dr. Sandhu then discussed the VISION trial, which was an international, randomized, open-label phase III study evaluating Lu-PSMA in men with PSMA-positive mCRPC who had previously received treatment with a next-generation androgen receptor signaling inhibition (abiraterone, enzalutamide, etc) and one or two prior lines of taxane chemotherapy.2 Patients must have had an ECOG performance status of 0-2 and life expectancy of at least 6 months. Importantly, patients must have had PSMA-positive disease on the basis of a central review of 68Ga-PSMA-11 staging scans. PSMA positivity was defined as uptake greater in metastatic lesions than in the liver. Further, they could have no PSMA-negative metastatic lesions. Following enrollment, patients were randomized in a 2:1 fashion to receive either Lu-PSMA (7.4 GBq every 6 weeks x 6 cycles) plus standard of care or standard of care alone. Standard of care treatments were at the discretion of the treating investigator; however, cytotoxic chemotherapy, immunotherapy, and radium-223 were explicitly excluded. Most patients received alternative androgen-directed therapies while others received palliative radiotherapy and glucocorticoids:

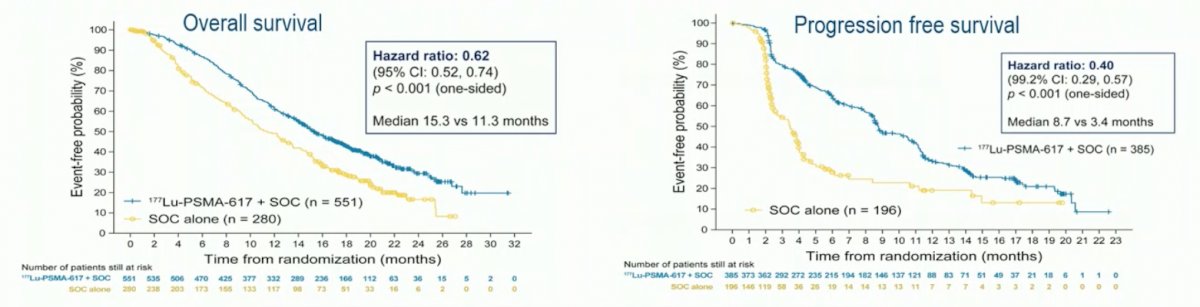
The authors assessed two alternate primary endpoints: (i) rPFS using the Prostate Cancer Working Group 3 (PCWG3) criteria by independent central review and (ii) OS. Secondary endpoints included ORR (RECIST v1.1), disease control rate, time to first symptomatic skeletal event, and safety/AE profile. VISION enrolled 831 patients between June 2018 and October 2019. In keeping with the 2:1 randomization schema, 551 patients were allocated to Lu-PSMA + standard of care, and 280 were allocated to standard of care only. Over a median study follow-up of 20.9 months, treatment with Lu-PSMA + standard of care significantly improved OS by a median of 4.0 months (median OS: 15.3 vs 11.3 months; HR 0.62, 95% CI 0.52 to 0.74; p < 0.001, one-sided), compared to standard of care alone, in the overall cohort of all randomized patients (n=831). With regards to the other primary endpoint of rPFS, treatment with Lu-PSMA + standard of care significantly improved rPFS by a median 5.3 months (median rPFS, 8.7 vs 3.4 months; HR 0.40, 99.2% CI 0.29 to 0.57; p < 0.001, one-sided):
Further, PSA responses (whether defined as a 50% decrease or an 80% decrease) were significantly more common among those treated with Lu-PSMA + standard of care:

Patient reported outcomes as evaluated by the FACT-P and Brief Pain Inventory (BPI) scores favored the Lu-PSMA arm with delays in time to worsening of 7.3 and 11.4 months, respectively:

While a higher rate of high-grade (grade 3-5) treatment-emergent adverse events was observed with Lu-PSMA (28.4% vs 3.9%) at the time of initial reporting, overall therapy was well tolerated. Adjusted safety analysis, accounting for a longer safety observation due to longer rPFS in patients receiving Lu-PSMA, revealed a comparable incidence of treatment-emergent adverse events between arms.
Importantly, from work presented at GU ASCO 2022, the magnitude of PSMA uptake has emerged as a predictive biomarker: in patients with PSMA SUVmean levels of 10 of greater, the odds of a response to Lu-PSMA were substantially higher (OR 12.2, 95% CI 3.4 to 59.0) as compared to those with PSMA SUVmean of less than 10 (OR 2.2, 95% CI 1.1 to 4.5) (p-value for difference = 0.03). This was reflected in superior PSA50 response rates (91% versus 52%):

Additional work from ASCO 2022 looking at rPFS by whole-body SUVmean quartiles showed that higher whole-body SUVmean was associated with improved clinical outcomes: those patients in the highest quartile (SUVmean: rPFS, ≥ 10.2; OS, ≥ 9.9) had a median rPFS and OS of 14.1 and 21.4 months, vs 5.8 and 14.5 months for those in the lowest quartile (< 6.0; < 5.7), respectively:

Furthermore, when assessing the association of these quartiles of whole body SUVmean with overall survival, again there was a significant stratification between the groups. Notably, among these patients who received Lu-PSMA, those with the highest SUVmean levels had the longest overall survival:

Dr. Sandhu notes that post-therapy imaging may better personalize care. At her institution, it is routine for patients to receive 24-hour qSPECT/CT scans to assess for response, thus potentially eliminating the necessity for subsequent Lu-PSMA doses. She notes that in TheraP, 7% of patients paused treatment owing to exceptional response recommenced upon progression:

What about Lu-PSMA therapy in patients with a superscan? Gafita and colleagues3 retrospectively assessed the efficacy of Lu-PSMA in 43 patients who received 154 cycles of Lu-PSMA. Median baseline PSA was 1,000 (interquartile range 431-2151) ng/ml. PSA decline of at least 50% at 12 weeks was achieved in 22 (58%) patients:

while median time to pain progression was 8.3 (95% CI 4.1-12.6) months, and median overall survival was 11.6 (95% CI 8.8-14.3) months. Objective response in nodal or visceral disease was reported in seven (39%) of 18 patients with RECIST measurable disease. Grade 3 anemia, thrombocytopenia, and neutropenia occurred in nine (22%), seven (17%), and three (8%) patients, respectively. Grade 4 thrombocytopenia was noticed in three (8%) patients.
What happens to men that were screened for a clinical trial but were not included secondary to low PSMA expression?4 Among 16 patients excluded, the median PSA doubling time was 2.1 months, all patients had previously progressed after docetaxel, 44% after cabazitaxel, and 94% after abiraterone and/or enzalutamide. Fifteen patients died, with a median OS of 2.5 month (95% CI 1.7-5.0).
Dr. Sandhu then provided the following practical overview of how Lu-PSMA planning and treatment administration is provided at her institution:

Dr. Sandhu concluded her presentation discussing Lu-PSMA for prostate cancer treatment with the following take-home messages:
- The use of Lu-PSMA in mCRPC is for men post-androgen receptor pathway inhibitor and post-taxane chemotherapy
- We should use PSMA PET to select patients. Recent works has suggested increased response rate with increased PSMA intensity
- It is important to have close collaboration of medical oncology, nuclear medicine, and include multi-disciplinary discussions
- Post-treatment 24-hour qSPECT/CT is cheap, accessible, and can assist with personalization of Lu-PSMA delivery
Presented by: Shahneen K. Sandhu, MBBS, FRACP, Peter MacCallum Cancer Centre, Melbourne, Australia
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 European Society for Medical Oncology (ESMO) Annual Congress, 9-13 September 2022.
References:
- Hofman MS, Emmett L, Sandhu S, et al. [(177)Lu]Lu-PSMA-617 versus cabazitaxel in patients with metastatic castration-resistant prostate cancer (TheraP): A randomized, open-label, phase 2 trial. Lancet. 2021 Feb 27;397(10276):797-804.
- Sartor O, de Bono J, Chi KN et al. Lutetium-177-PSMA-617 for Metastatic Castration-Resistant Prostate Cancer. N Engl J Med. 2021 Sep 16;385(12):1091-1103.
- Gafita A, Fendler WP, Hui W, et al. Efficacy and Safety of 177Lu-labeled Prostate-Specific Membrane Antigen Radionuclide Treatment in patients with diffuse bone marrow involvement: A multicenter retrospective study. Eur Urol. 2020 Aug;78(2):148-154.
- Thang SP, Violet J, Sandhu S, et al. Poor outcomes for patients with metastatic castration-resistant prostate cancer with low prostate-specific membrane antigen (PSMA) expression deemed ineligible for 177Lu-labelled PSMA radioligand therapy. Eur Urol Oncol. 2019 Nov;2(6):670-676.