(UroToday.com) In this study, Dr. Neal Shore and colleagues evaluate the impact of late dosing on testosterone suppression with two different leuprolide acetate formulations: In situ gel and microsphere.
Luteinizing hormone-releasing hormone (LHRH) agonists are the most frequently used drugs for the delivery of androgen deprivation therapy (ADT) in prostate cancer (PCa). Achieving and maintaining effective testosterone (T) to the levels attained with surgical castration is the cornerstone of ADT for advanced PCa. However, T levels may rise above castrate level (50ng/dL) between injections, especially if a subsequent dose is delayed – and this may have an impact on prostate cancer outcomes as non-castrate levels can promote clonal growth of prostate cancer.
A large US analysis of LHRH agonists confirmed that late dosing is common (27%). Late injections were associated with a 4x higher T breakthrough rate and doubled mean T compared to early/on-time injections. Therefore, delivery systems should be considered. Two FDA approved forms of leuprolide acetate (LA), the most commonly used LHRH agonist in the US, use different extended-release systems: in situ gel technology (Gel-LA, subcutaneous) and microsphere technology (Msphere-LA, intramuscular). This study evaluated the prevalence of late dosing and comparative impact of late dosing on T suppression for Gel-LA and Msphere-LA.
This was an observational analysis (1/1/07-6/30/16) of US oncology and urology electronic medical records of PCa patients who received Gel-LA or Msphere-LA injections, evaluated for frequency of late dosing (occurring after day 32, 97, 128, 194 for 1-, 3-, 4-, 6-month formulations, respectively), mean T and rate of T tests >50/20ng/dL with late dosing.
They identified 2,038 patients who received Gel-LA and 8,360 who received Msphere-LA.
Demographics are below: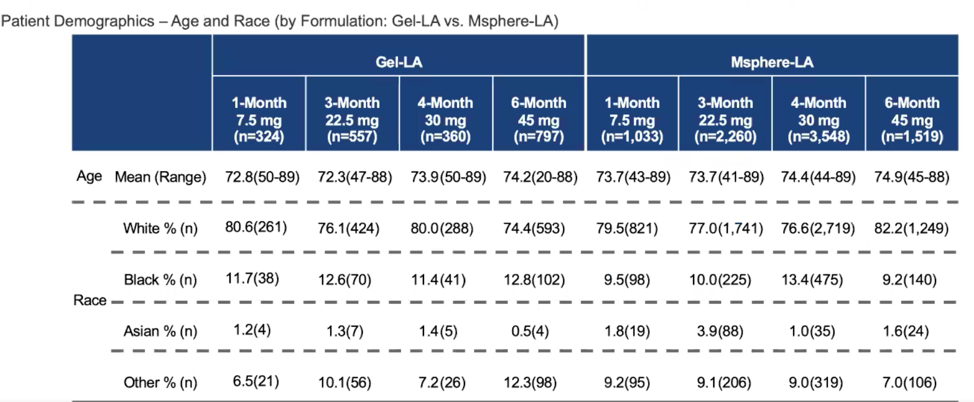
27% of injections for both drugs were late. Data on late dosages is below: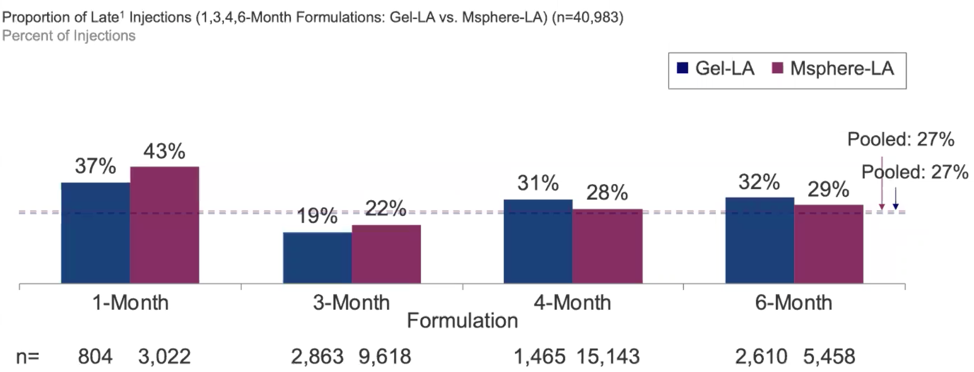
When dosing was late, mean T was 48ng/dL (Gel-LA) vs. 76ng/dL (Msphere-LA), and 18% (Gel-LA) vs. 25% (Msphere-LA) of T values were >50ng/dL. Both of these analyses were statistically significant (p<0.05). 34% (Gel-LA) vs. 44% (Msphere-LA) of T values were >20ng/dL (p<0.05).
Based on this, they conclude that more than a quarter of injections were late. With late injection, Gel-LA showed higher rates of T suppression than Msphere-LA, demonstrated by lower rates of T above 50/20ng/dL and lower mean T. Although modifying clinical practice procedures to increase adherence to dosing schedules is recommended, late injections are ubiquitous in real world practice. As higher T levels, including T escapes, have the potential to adversely impact disease progression and survival, clinicians should reassess their dosing schedule compliance policies and use an ADT that optimizes the goal of effective T suppression to castrate levels.
Presented by: Neal D. Shore, MD, FACS, Carolina Urologic Research Center. Myrtle Beach, South Carolina.
Written by: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Assistant Professor of Urology, Sidney Kimmel Cancer Center, Thomas Jefferson University, @tchandra_uromd on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.


