Lymphatic drainage of penile cancer – similar to testicular cancer, it is well established. Drainage goes from glans, corpora, and skin to the (bilateral) superficial inguinal nodes, then deep inguinal nodes, and then pelvic nodes.
What is the relevance of inguinal nodes?
- Inguinal node status is the strongest prognostic indicator in penile cancer. Node positive patients do very poorly (25-40% 5-year survival), but node-negative patients do very well (85%+ 5 year survival).
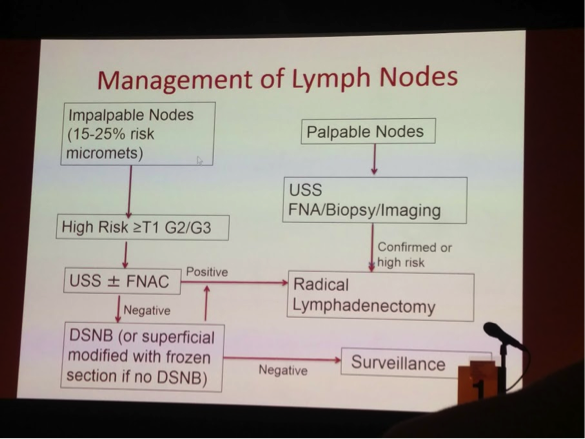
- Patients with cN0 disease still have a 12-25% risk of occult inguinal node positivity – hence the need to do a node dissection in high risk patients
o High risk defined as pT1G2 or higher
- Node dissection may be curative
o pN1 patients after node dissection have 80-90% 5-year survival, but those that are pN2+ have <20% 5-year survival
How do we manage cN0 disease?
1. Clinical surveillance
- Potential to miss micrometastases in those who would benefit from early LND
- Long term patient compliance is poor
- Unreliable surveillance tools
- Clinical exam sensitivity: 40-60%
- USS/FNA sensitivity: 39%
- CT/MRI sensivity: <50%
Therefore, we take a risk-adapted approach. Goal is maximize cure and minimize morbidity.
2. Radical inguinal node dissection
- appropriate for high stage, high-grade or palpable nodes
- highly morbid with a lot of potential complications – wound healing, seroma, edema, etc.
3. Superficial modified inguinal node dissection
- Catalona 1998 – introduced the modified template (no dissection lateral to the femoral vessels, smaller incision). Significantly less morbidity. Must be combined with on-table frozen sections – if positive, radical dissection needed.
- Only appropriate for cN0 patients
- Still has a 15% recurrence rate
4. Dynamic sentinel lymph node biopsy
- Dr. Muneer has experience with this – but clearly stated it has a steep learning curve
- The NKI (Amsterdam) helped advance this in its early days
- Combination of a 99mTc nanocolloid + gamma probe as well as a blue dye
- False negative rate (2001-2004) was 4.8%. Previously had been as high as 20%.
- Sadeghi JUrol 2012 – meta-analysis of 18 studies. Highest success when combining radiotracer + dye. Pooled sensitivity was 92%.
He then briefly reviewed the protocol for the procedure.
Their institution’s protocol for ILND is as follows:
He briefly alluded to newer attempts at robotic/MIS node dissection, which show early promising results, but oncologic outcomes are still not long-term.
Speaker: A. Muneer
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 2018 European Association of Urology Meeting EAU18, 16-20 March, 2018 Copenhagen, Denmark