Indications for no neoadjuvant chemotherapy include:
- WHO or ECOG PS of 2 or Karnofsky PS of 60-70%
- Creatinine clearance (calculated or measured) < 60 ml/min
- CTCAE v4 grade ≥2 audiometric hearing loss
- CTCAE v4 grade ≥2 peripheral neuropathy
- NYHA class III heart failure
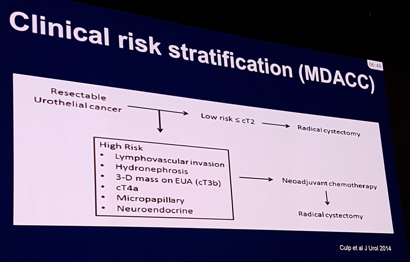
Patients that are cN+ should all be treated with upfront chemotherapy. Dr. Black notes that this is induction chemotherapy and not neoadjuvant chemotherapy and should be for 4 and sometimes 6 cycles. Surgery may play a role in this setting in two cases (i) consolidative surgery (or radiotherapy) if there is an appropriate response, and (ii) if platinum-ineligible, consider surgery if there is lower volume nodal disease, since not all of these patients are pN+. The MD Anderson Cancer Center clinical risk stratification has been used and validated in a USC cohort:
Variant histology includes most commonly micropapillary, sarcomatoid and plasmacytoid. These entities have a high risk of micrometastasis and upstaging, however there is uncertainty whether chemotherapy is effective. Dr. Black considers it reasonable to proceed with cystectomy without neoadjuvant chemotherapy if the patient is cT2-cTaN0M0 with variant histology. With regards to molecular markers to predict response to neoadjuvant chemotherapy, the EAU guidelines state that currently there are no tools available to select patients who have a higher probability of benefiting from neoadjuvant chemotherapy.
Dr. Black concluded with several take-home messages: (i) cisplatin-ineligible patients should not receive neoadjuvant chemotherapy, (ii) otherwise cisplatin-based neoadjuvant chemotherapy is default for all non-metastatic MIBC, (iii) clinical risk stratification is imperfect, but neoadjuvant chemotherapy is less important in lowest risk patients, and (iv) molecular markers will soon guide the use of neoadjuvant chemotherapy.
References:
1. Grossman HB, Natale RB, Tangen CM, et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med 2003;349(9):859-866.
Presented by: Peter C. Black, Vancouver Prostate Centre, Vancouver, BC, Canada
Written by: Zachary Klaassen, MD, Urologic Oncology Fellow, University of Toronto, Princess Margaret Cancer Centre, twitter: @zklaassen_md at the 2018 European Association of Urology Meeting EAU18, 16-20 March, 2018 Copenhagen, Denmark