To that effect, of their entire TCa database, they identified 267 men between 1981 and 2016 who had adequate records for analysis and had documented prior inguinoscrotal surgery (including orchiectomy, orchiopexy, varicocelectomy, hydrocelectomy, scrotal violation at the time of orchiectomy, etc); 141 men had seminoma (SEM) and 126 had non-seminomatous germ cell tumors (NSGCTs). This was primary a descriptive study of the patient's diagnosis, management and recurrence patterns.
The two flow diagrams below highlight the breakdown of patients by histology:
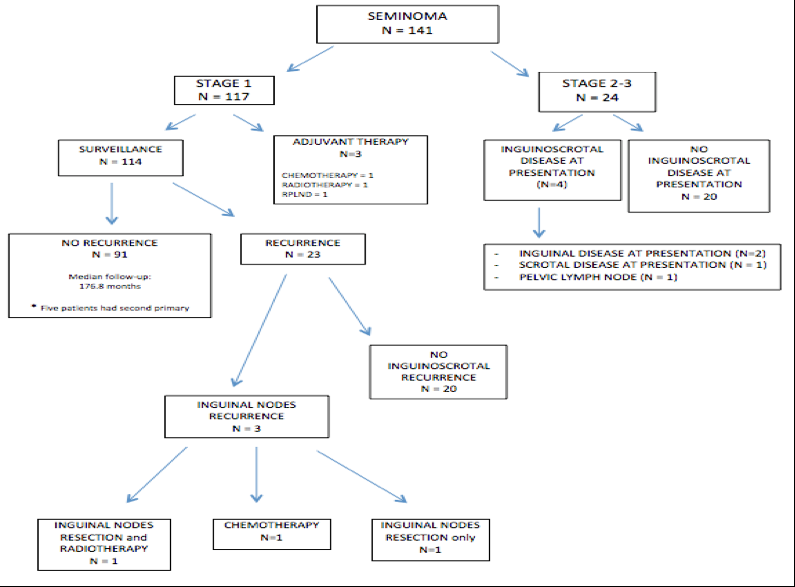
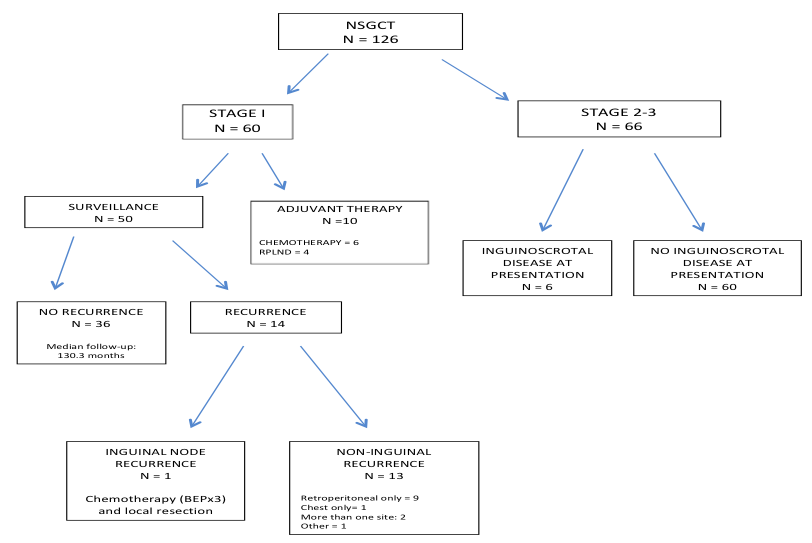
Looking at the entire cohort, inguinoscrotal recurrence occurred in 2.3% of men with CSI TCa (4/177). This was isolated inguinoscrotal recurrence 1.7% (3/177).
Of all men who presented with metastatic TCa, inguinoscrotal recurrence was identified in 11.1% (10/90). Isolated inguinoscrotal disease was identified in 2.2% (2/90) of those men.
Prior orchiopexy appeared to be the predominant risk factor for inguinoscrotal recurrence amongst AS patients, regardless of histology (6.2% of seminoma patients and 5.6% of NSGCT patients developed inguinoscrotal recurrence on AS).
In terms of diagnosis, when looking at how men with inguinoscrotal recurrence were diagnosed, recurrences were identified on staging imaging studies (n = 13, 92.9%) or on exam (n = 12, 85.7%). Only in 1 patient was the recurrence identified on exam alone. Hence, staging studies (including pelvic imaging) remain an important method of detection. As more recent AS algorithms have begun to exclude pelvic imaging later in follow-up, perhaps in this population it may be warranted to include pelvic imaging for continued follow-up?
As can be expected, survival outcomes remained high. With a mean follow-up of 5 years, disease-free survival rates for patients with seminoma and NSGCT on active surveillance were 98.2% and 98.0% respectively. All 4 patients on AS with inguinoscrotal recurrence continue to be followed without evidence of recurrence.
Based on this, the authors conclude that the risk of inguinoscrotal recurrence for patients with prior ISS on surveillance for TCa remains low, consistent with historical series, and disease-specific survival remains high. However, inguinoscrotal recurrence may be an early harbinger of systemic spread. As such, pelvic imaging on surveillance protocols should be maintained for patients with prior ISS for the entire duration of their follow up. Consideration should be given to systemic chemotherapy in cases of recurrence.
Limitations / Discussion Points:
1. There is no comparison to men who did not have inguino-scrotal recurrence – per the authors, a lack of documentation of ISS does not mean the remaining patients didn’t have one. As this could not be assured, this comparison wasn’t done.
Presented by: Dixon T. Woon, MD, Uro-oncology Fellow, University of Toronto, Toronto, Canada
Co-Authors: Thenappan Chandrasekar, Jaime Omar O. Herrera Cáceres, Hanan Goldberg, Zachary Klaassen, Neil Fleshner, Michael Jewett, Robert Hamilton.
Written by: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto, Twitter: @tchandra_uromd at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia