For the purpose of this study, the Delayed Intervention and Surveillance for Renal Masses (DISSRM) registry prospectively enrolled 739 patients since 2009; 374 elected active surveillance (AS). Patients undergoing AS with at least one surveillance image showing no tumor, were considered to have a DRT. Multivariable logistic regression analysis assessed predictors of DRTs and Kaplan Meier estimates measured survival.
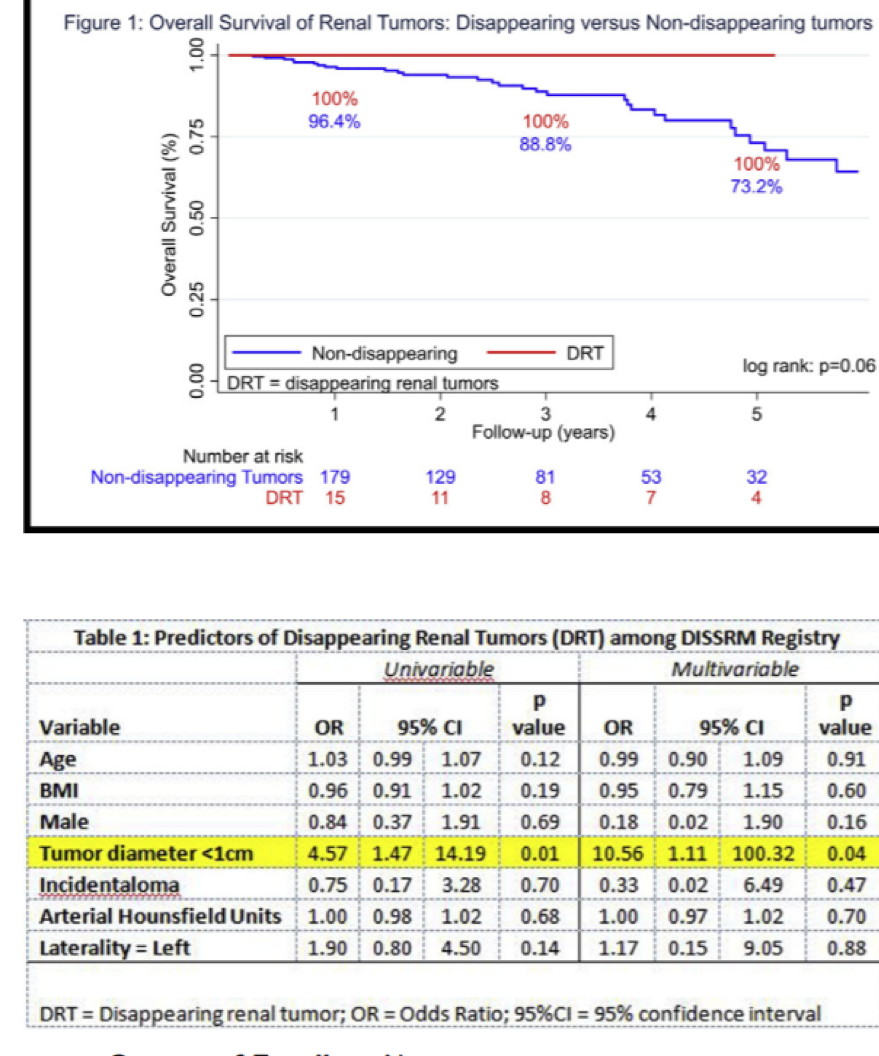
Of 374 AS patients, 22 (5.9%) experienced a DRT in their follow-up imaging. Average time to DRT disappearance was 1.2 years and 54.5% of tumors reappeared on subsequent CT imaging (12/22). Of the 22 DRT cases, 15 were produced by ultrasound, 5 by CT scan, and 2 by MRI. Of the 15 DRT on ultrasound, 7 (46.7%) were picked up on subsequent axial imaging. Univariate and multivariable analyses demonstrated that tumor diameter <1 cm significantly predicted DRT among the entire cohort (OR = 10.6, p=0.04) (Table 1). Lastly, DRT patients may have improved outcomes versus other AS patients (5 year survival of 100% vs. 73.2%, p = 0.06) (Figure 1).
In a large prospective AS cohort, the authors found that approximately 5% of patients will experience a DRT. This most often occurs when using ultrasound modalities and with small tumors <1cm. However, this does not necessarily mean that the tumor has disappeared, as approximately 50% will be visible on subsequent imaging. However, a DRT may imply low biological risk and may not require immediate axial imaging if tumor size is small. Further studies should validate this assumption.
Presented by: Arnav Srivastava, James Buchanan Brady Urological Institute, Johns Hopkins Medical Institutions, Baltimore, MD, USA
Co-Authors: Hiten Patel, Mohit Gupta, Gregory Joice, Zeyad Schwen, Ridwan Alam, Michael Gorin, Michael Johnson, Mohamad Allaf, Phillip Pierorazio, Baltimore, MD
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 AUA Annual Meeting - May 18 - 21, 2018 – San Francisco, CA USA