Dr. Ziad Bakouny et al. retrospectively reviewed the International Metastatic RCC Database Consortium to evaluate the role of CN for patients with mRCC treated with ICI or TT using a propensity score-based analysis. All patients assessed were diagnosed with de novo mRCC and were treated with first-line systemic therapy via ICI or TT. The investigators compared overall Survival (OS) between patients receiving CN and systemic therapy versus patients receiving systemic therapy alone. More specifically, the comparison was made using the Kaplan-Meier method and Cox regressions in the ICI and TT arms separately. In order to account for treatment selection bias, inverse probability of treatment weighting (IPTW) of propensity scores, based on 14 confounding variables, was used and variables were considered balanced if standardized mean difference (SMD) <0.1. This was particularly important to adjust for selection bias with regards to CN. For variables with SMD ≥0.1, residual confounding was adjusted for using multivariable models.
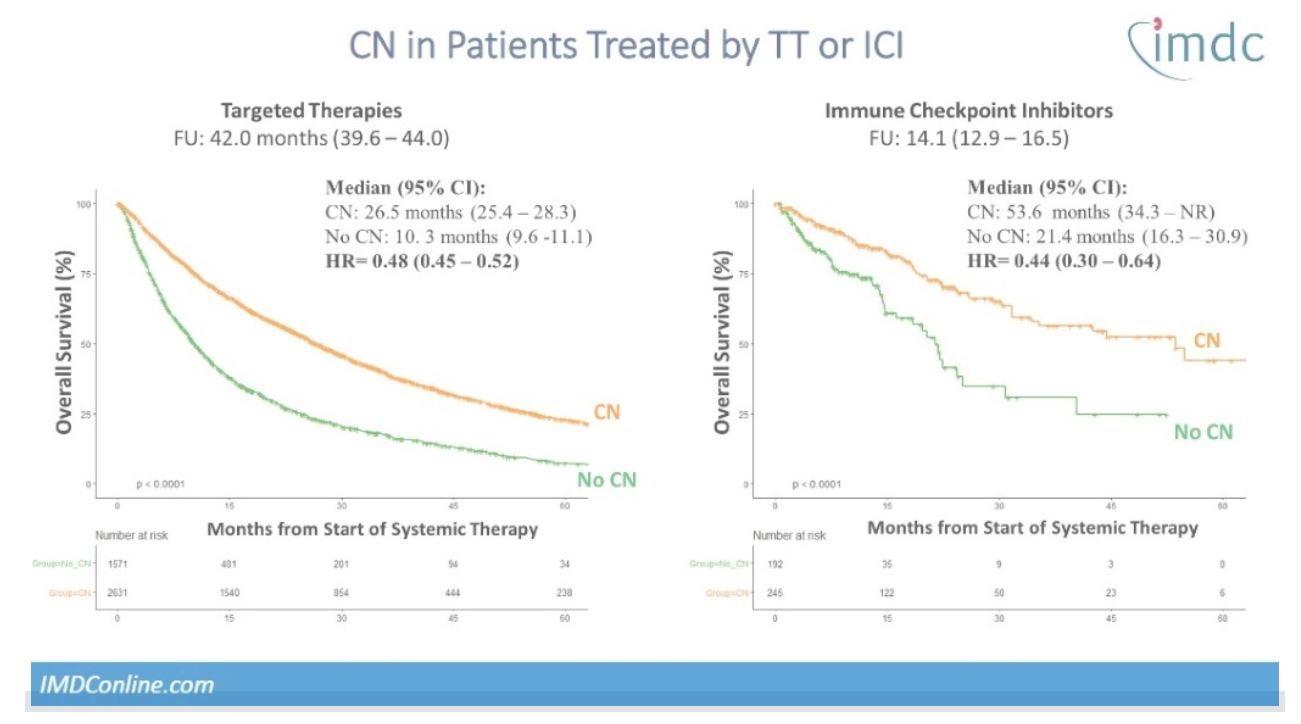
There were 198 patients treated with ICI (143 in the CN group and 55 in the ICI only group) and 3856 patients treated with TT (2470 in the CN group and 1386 in the TT only group). The overall median follow-up was 38.5 months. After IPTW, baseline characteristics were largely balanced between the CN + ICI versus ICI only groups (12/14 variables with SMD <0.1), and the CN + TT versus TT only groups (14/14 variables with SMD <0.1). The investigators noted an improved OS in patients in the CN + ICI group compared to ICI only group (53.6 versus 21.4 months, respectively; HR = 0.44), and in patients in the CN + TT group compared to TT only group (25.4 versus 10.3 months, respectively; HR = 0.48). The interaction term between CN and systemic therapy type (ICI versus TT) was not statistically significant (p = 0.43).
OS curves by treatment type are shown:
Dr. Bakouny concluded that in this propensity score-based analysis, CN was found to be associated with a significant OS benefit in patients treated by either ICI or TT. Although he acknowledged that this study was limited by its retrospective nature, he emphasized that CN may still play a role in selected patients in the ICI era.
Presented by: Ziad Bakouny, MD, MSc, Postdoctoral Genitourinary Oncology Research Fellow, Dana-Farber Cancer Institute, Boston, Massachusetts
Written by: Ziho Lee, MD,Fellow in Advanced Robotic Oncology and Reconstruction, Temple University, Philadelphia, PA, Twitter: @ZLeeGU at the 2020 Genitourinary Cancers Symposium, ASCO GU #GU20, February 13-15, 2020, San Francisco, California
References:
1. Mejean A, Ravaud A, Thezenas S, et al. Sunitinib Alone or after Nephrectomy in Metastatic Renal-Cell Carcinoma. N Engl J Med. 2018;379:417-427.



