- Oncologic efficacy
- Preservation of renal function
- Reduction of perioperative morbidity
- Cosmesis
The only prospective study published comparing the oncologic outcome of PN vs. RN in low stage RCC, was the EORTC 30904, published in 2011.3 It included 541 patients randomized from 45 institutions and 17 countries between 1992-2003. The primary endpoint was overall survival (OS) and all patients had tumors smaller than 5 cm. On intention to treat (ITT) analyses there was a 10 year OS of 75.7% for PN an 81.1% for RN, with a hazard ratio (HR) of 1.5, p=0.03 (Figure 1).
The EORTC 30904 study has several known limitations. These include the low accrual rate, lack of information on the amount of parenchyma preserved, quality of PN performed, and high crossover from the PN to the RN group (15%).
An analysis of the EORTC trial 30904 study was performed in an attempt to compare renal function between PN and RN. However, the comparison was done only based on creatinine levels. The results demonstrated that PN had less incidence of moderate CKD, the incidence of advanced CKD and renal failure were the same. However, the OS was better for RN than for PN.
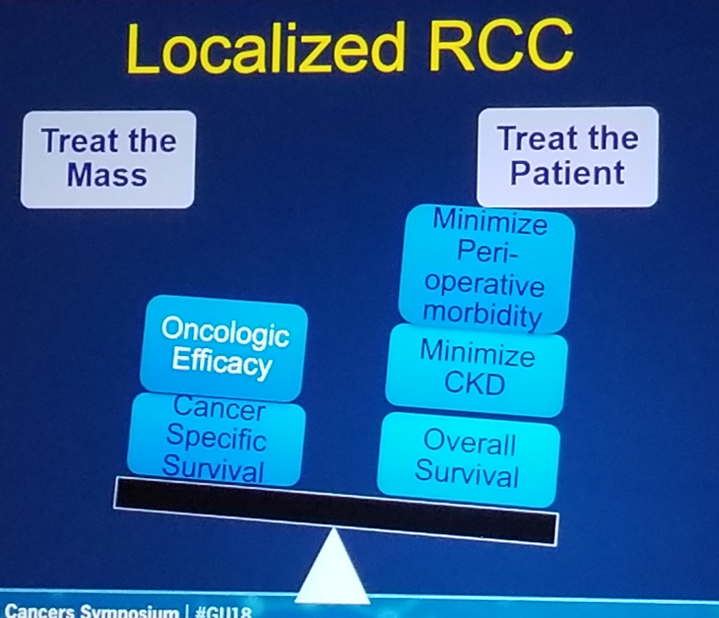
Dr. Parikh continued his talk and stated that the EORTC 30904 was a well intentioned but poorly accrued randomized controlled trial. Therefore, he does not think this study provides level 1 evidence for choosing one form of therapy over the other. In treating these patients, there is always a dilemma of treating the mass or treating the patients (Figure 2).
Dr. Parikh moved on to his recommendations regarding treatment of localized RCC with a normal contralateral kidney:
- For T1a – PN
- For T1b – PN or RN and we should consider tumor/patient factors and surgeon experience
- For T2 – RN/PN and we should consider tumor/patients factors and surgeon experience
- For T3-T4 – RN
Figure – 1: Overall survival comparison between radical nephrectomy and partial nephrectomy:
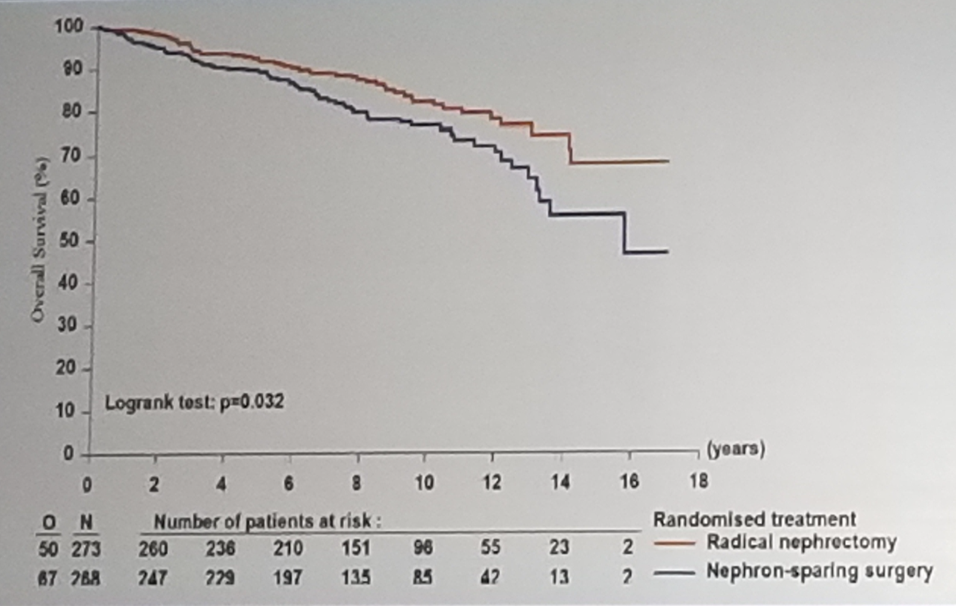
Figure 2 – Treating the patient or the tumor mass:
Presented by: Dipen J. Parekh, MD, University of Miami Miller School of Medicine
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 2018 American Society of Clinical Oncology Genitourinary (ASCO GU) Cancers Symposium, February 8-10, 2018 - San Francisco, CA
References:
1. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C-y. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. New England Journal of Medicine 2004; 351(13): 1296-305.
2. Huang WC, Levey AS, Serio AM, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. The Lancet Oncology 2006; 7(9): 735-40.
3. Van Poppel H, Da Pozzo L, Albrecht W, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. European urology 2011; 59(4): 543-52.


