Dr. Nicholas James began his discussion of the case noting that technically this patient has M0 disease by traditional definition, and therefore the role of radiotherapy really applies in the context of previous trials such as PRO-7 and SPCG-7, which examined the role of endocrine therapy in combination with radiotherapy for locally advanced prostate cancer. It is likely that many patients on those trial would have had PSMA-PET evidence of metastatic disease. Based on those two trials, which demonstrated a statistically significant reduction in prostate cancer mortality with the addition of radiation to the primary tumor on top of endocrine therapy, the default for this patient should be direct treatment of the prostate tumor. He then discussed the STAMPEDE data1 showing a benefit to radiotherapy to the prostate (prostate only, not pelvic nodes) in metastatic prostate cancer proven by conventional imaging, so long as the metastatic burden is considered low volume by CHAARTED criteria.
An audience question was posed regarding whether all patients with high-risk prostate cancer should undergo PSMA-PET. Dr. James commented that by doing so, you enter a decision-making realm that is not studied by the current prostate cancer treatment literature. However, as people are doing this test more and more, he feels that PSMA-PET is likely to be yielding useful information, and if you discover low volume metastatic disease by PSMA-PET, then a combination of androgen deprivation therapy, a newer androgen receptor signaling pathway inhibitor, and treating the primary prostate tumor as well as metastatic sites together is likely indicated.
Regarding whether the three osseous metastatic lesions seen in this patient can be treated with benefit, Dr. James discussed a recent paper from the STAMPEDE group showing that the benefit of therapy to oligometastatic bone lesions likely is associated with a survival benefit if up to five metastatic lesions are present.
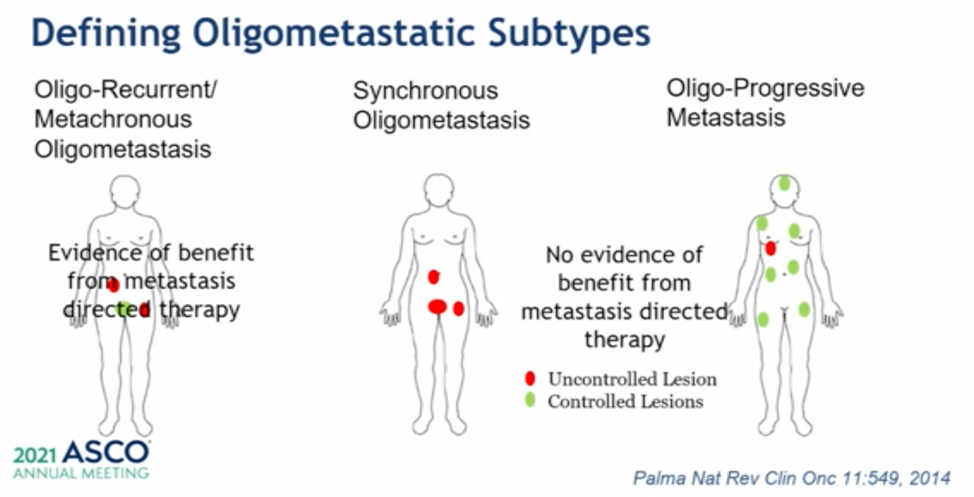
He then shared a published potential classification of oligometastatic disease subtypes, which is shown below. There is evidence of benefit to metastasis-directed therapy in metachronous oligometastatic disease (previously treated primary, then disease recurs in an oligometastatic fashion) from the STOMP and ORIOLE trials, which showed a delay in time to needing systemic therapy subsequently. He concluded this case discussion by suggesting that there is no clear prospective evidence of how best to manage synchronous oligometastatic disease, though many would treat with androgen deprivation therapy, an anti-androgen signaling inhibitor, treatment to all metastatic sites, and treatment to the primary prostate lesion.
Case 2: 66M who underwent robotic prostatectomy and standard pelvic lymph node dissection for pT2cN0M0 Gleason 4 + 4 adenocarcinoma. Post-op PSA was detectable at 0.04 and rose to 1.0 over the next year. CT and bone scan were negative, but a sodium fluoride PET scan showed a bony metastatic lesion to the 9th right rib. The patient was treated with 3000 cGy to the rib with a short course of androgen deprivation therapy. After two years of undetectable PSA, the patient’s PSA rose to 1.6 ng/mL. A fluciclovine PET/CT was obtained, which showed a left pelvic nodal area of avidity.
Dr. James noted that as we are doing more prostate-specific PET imaging, we are often detecting avid areas of lymph nodes that are not associated with pathologic enlargement by size criteria and are not in the typical drainage area for the prostate.
An audience member posed the question of whether androgen deprivation therapy is essential in combination with radiation therapy for nodal relapsed disease, and for how long. Dr. James mentioned that it is important to think about this fluciclovine-PET finding in the context of what we know from evidence using conventional imaging. In this case, this patient would have biochemical recurrence without known M1 disease, a context in which many patients would receive intermittent hormonal therapy. Additionally, he emphasized that the long-term toxicity of ADT is not benign, so if you can postpone ADT for a period of time by using radiotherapy alone, this would be his preference.
Another audience question to Dr. James was regarding the robustness of the conclusion of radiation to the primary in low volume metastatic castration sensitive prostate cancer as this analysis within STAMPEDE was a subgroup analysis. Dr. James responded that a few things lend support to this being a plausible finding despite it being a subgroup. It was a pre-specified analysis, and there were similar trends noted in both failure-free survival and overall survival. Furthermore, a test for interaction between the administration of radiotherapy and disease volume revealed that the high and low volume subgroups had a statistically significant differential response to radiotherapy. Finally, he noted that this study was published in Lancet, which requires an independent statistical review of studies.
Case 3: 66M with cT2cN1M0 Gleason 5+4 in 12/12 biopsy cores, PSA 14 ng/mL who was initially treated with radiotherapy and long-term ADT. For two years after initial therapy, his PSA remained in the 0.7-1.3 ng/mL range, but then rose to 5.4 ng/mL despite testosterone level less than 20. Imaging showed new bulky > 2.5 cm left-sided para-aortic and RP nodes.
The potential options polled to the audience for management at this juncture were sipuleucel-T (which is not available in many countries), abiraterone, docetaxel, enzalutamide, and lutetium-177. Most respondents chose either abiraterone or enzalutamide. Dr. James discussed that there is not a lot of data to help discriminate between the two (at least from an overall survival perspective) so he tends to choose based on age (younger, fitter patients more often get enzalutamide), or comorbidities (risk of uncontrolled hypertension with abiraterone).
Presented by: Nicholas D. James, PhD, MBBS, FRCP, Medical Oncologist
Written by: Alok Tewari, MD, PhD, Medical Oncologist at the Dana-Farber Cancer Institute, at the 2021 American Society of Clinical Oncology (ASCO) Annual Meeting, Virtual Annual Meeting #ASCO21, June, 4-8, 2021
References:
- Christopher C Parker, Prof Nicholas D James, Christopher D Brawley, et al. "Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial." The Lancet. 2018. 392, 10162, P2353-2366.
- Adnan Ali, Alex Hoyle, Áine M. Haran, et al. "Association of Bone Metastatic Burden With Survival Benefit From Prostate Radiotherapy in Patients With Newly Diagnosed Metastatic Prostate Cancer." JAMA Oncol. 2021;7(4):555-563.


