This was a retrospective analysis using propensity score matching performed on 1,503 IRPC patients treated in a single center, who were treated from 2004 to 2007. Overall, 819 patients underwent RP, 574 underwent EBRT to a median dose of 75.3 Gray, and 110 underwent BT using iodine-125.
The median follow-up was time was 10.0 years for RP patients, 9.6 for EBRT, and 9.8 for BT (range 1.0-13.4 years). When assessing the Gleason scores:
76.3% of the RP patients had Gleason score 7 vs 72.8% for EBRT vs 57.3% for BT, p = 0.0001. Median initial PSA was 7.4 for RP, 9.4 for EBRT, and 8.3 for BT, p < 0.0001. Importantly, neoadjuvant androgen deprivation therapy (ADT) was given to 58.9% of EBRT patients vs 12.7% of BT vs. only 0.6% for RP, p < 0.0001. An additional 14% of BT received supplemental external radiation.
When assessing the results, the 10-year freedom from biochemical failure (FFBF) was 82.0% for BT vs 58.0% for RP vs 58.8% for EBRT, p < 0.0001 (Figure 1).
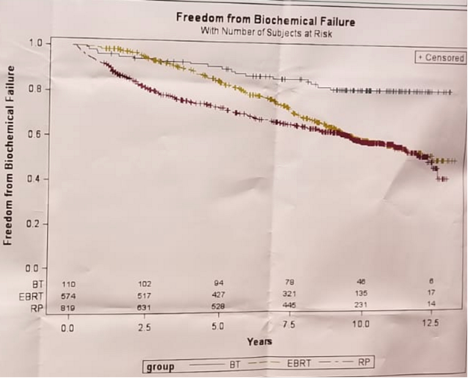
The authors also performed subset analysis of unfavorable IRPC patients. This demonstrated a 10-year FFBF of 81.6% for BT vs 55.8% for RP vs 51.0% for EBRT, p < 0.0001. The 10-year freedom from salvage therapy was 89.5% for BT vs 64.0% for RP vs 73.4% for EBRT, p < 0.0001. Several outcomes had no significant differences. These included distant metastases-free survival, prostate cancer-specific survival, and overall survival.
The authors concluded that brachytherapy is a good therapeutic option for IRPC patients. Despite demonstrating improved FFBF for BT patients after propensity score matching, this did not impact overall survival.
Although this study analyzed a large cohort of patients, there are significant limitations. These include the single center retrospective nature of it leading to the obvious selection bias, and the fact that the BT patients probably had less aggressive disease due to the lower Gleason 7 percentage of patients. Furthermore, only 0.6% of RP patients received ADT compared to much high number in the radiotherapy patients. Additionally, no data is given on the duration of ADT. No significant difference was shown between patients treated with EBRT and RP, similarly to other large prospective published studies.
Presented by: Barry W. Goy, Kaiser Permanente Los Angeles Medical Center, Los Angeles, CA
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the 2018 ASCO Annual Meeting - June 1-5, 2018 – Chicago, IL USA


